1591
Ultra-Flexible, High-Resolution, 60-Channel RF Coil for Supine Breast Imaging1GE Healthcare Coils, Aurora, OH, United States, 2Weldon School of Biomedical Engineering, Purdue University, West Lafayette, IN, United States, 3Basic Medical Sciences, Purdue University, West Lafayette, IN, United States, 4Global MR Applications & Workflow, GE Healthcare, Houston, TX, United States, 5Global MR Applications & Workflow, GE Healthcare, Waukesha, WI, United States, 6Global MR Applications and Workflow, GE Healthcare, Madison, WI, United States, 7Albert Einstein College of Medicine, Montefiore Medical Center, Bronx, NY, United States, 8Center for Advanced Imaging Innovation and Research, Department of Radiology, NYU School of Medicine, New York, NY, United States, 9GE Healthcare, Waukesha, WI, United States, 10School of Electrical & Computer Engineering, Purdue University, West Lafayette, IN, United States
Synopsis
Typically, breast MR scans are performed prone; however, there are advantages to supine imaging. Here we present the first 60-channel, high-resolution, flexible breast coil. The coil can be run with the embedded posterior coil for a total of 90-channels in the FOV. In addition to better image quality, with such a high channel count, an acceleration of up to 5 by 2 was possible. Due to the structured shape, breast tissue was kept in place for the duration of the scan and women with cup sizes up to a DD could be accommodated. Straps provide adjustments for smaller bust sizes.
Introduction
While mammography remains as the conventional method for breast screening, Magnetic Resonance Imaging (MRI) has been shown to have greater sensitivity and is recommended for supplemental screening, especially in cases of patients with denser breast tissue or greater risk of breast cancer1,2. Breast MRI screenings are typically performed in the prone position, which allows for uncompressed tissue imaging and biopsy. However, physical breast examinations, ultrasound-guided biopsy, and surgery are performed in the supine position. The positional changes between prone and supine leads to changes in lesion localization, which is one of the challenges faced in surgical planning based on MRI-detected lesions3-5. There is also the challenge of coverage and patient comfort with existing prone radiofrequency (RF) coils. These coils are mechanically bulky and rigid, leading to discomfort along pressure points, while the prone positioning can, generally, be uncomfortable for those with musculoskeletal weakness, advanced age, or increased weight with pressure on the sternum. In addition, level III axillary lymph nodes and supraclavicular lymph nodes are not always encompassed by the conventional coil. Supine breast imaging has shown promise in alleviating these discomforts while providing more accurate positioning for surgical or radiation therapy planning5,6. In this paper, a novel, flexible, high-resolution, high-channel breast coil is presented for small to large sized patients. This prototype was constructed on fabric materials, encompassing a bust size of up to 40 DD and was evaluated on phantoms as well as asymptomatic human volunteers under an IRB-approved protocol.Methods
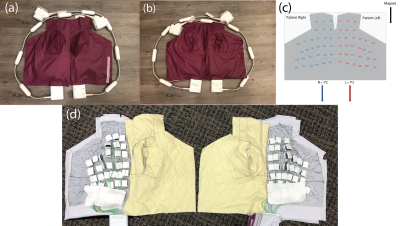
A novel, 60-channel, bilateral, supine breast array was developed using 7-cm diameter highly overlapped elements and flexible fabric materials based upon AIR™Coil technology7,8. These specific loops are made from highly flexible, 1.3-mm diameter conductor optimized for zero reactance at 127.73 MHz. The electronics module includes a preamplifier, active and passive decoupling, matching circuitry and baluns. Coil preamplifier decoupling is controlled by the use of custom E-mode preamplifier7,8. The final coil assembly was designed to accommodate a structured contour of bust sizes up to DD, while providing coverage of the axilla, breast, and supraclavicular lymph nodes (Fig.1). The coil elements are between two, 1-mm thermoplastic coated fabrics with a medical grade sleeve for biocompatibility and a water seal, making the whole package easily cleanable. The coil was developed and tested on a 144-channel 3T GE Premier scanner (Signa Premier, GE Healthcare, Aurora, Ohio USA). To test the conformability and sensitivity of the coil during design optimization, a novel compartmentalized breast coil phantom9 was used in combination with a rectangular phantom to simulate the female torso (Fig. 2). The 60-channels are distributed across each half of the chest and provide lightweight, adaptable coverage. The coil supports a R/L acceleration factor of 6 and S/I acceleration of 2 for typical breast coverage. In addition to the 60-channels, this coil can be run with an additional 30-channels of the embedded posterior coil. We ran the following sequences to evaluate the coil performance: SSFSE, LAVA Flex, and 3D Cube Flex.Results
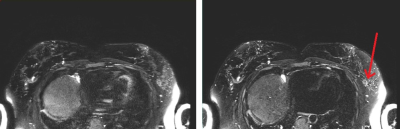
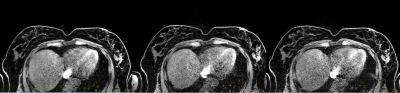
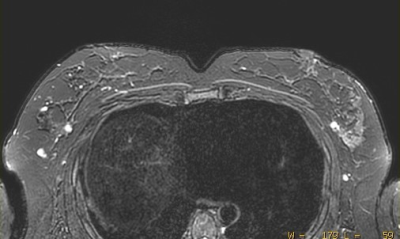
The unloaded phantom images were acquired with a spin echo sequence. Coil elements were found to be highly decoupled from each other even though the density of elements was extremely high. In both respiratory-gated and free breathing scans, axilla/chest wall visualization was clear in the presence of motion. SSFSE, LAVA Flex, and 3D Cube Flex images are presented in Fig.3-5, respectively.Discussion
The coil was found to be flexible, easy to use, and provided significant improvement in image quality. The coil allows mitigation of respiratory and motion artifacts through high acceleration which is made possible with the high channel count and commensurate SNR, which in turn facilitates supine breast imaging.Conclusion
This novel, 60-channel, supine breast and female torso coil can accommodate chest sizes up to 40 DD with ultra-flexibility, comfort, high-resolution and high-acceleration imaging with the lightweight miniaturized electronics, exceptionally low-noise preamplifiers, and overall lightweight, wearable mechanical construction. This coil provides an enhanced degree of comfort over prone positioning and greater coverage of lymph nodes than existing breast coils. The axillary lymph nodes and supraclavicular lymph nodes can also be visualized. The increased acceleration provides faster imaging time, while the coil design contributes to reduced coil setup time and improves patient compliance. We intend to further test this coil on a wider range of body habitus, push acceleration further, and explore the use of the coil for female cardiac and abdominal images. The use of additional breast supports is being explored.Acknowledgements
The authors would like to thank Anja Brau, Bruce Daniels, Katja Pinker-Domenig, Fiona Gilbert, and Bahar Behzadnezhad for inspiration and Kris Barnhart and Ann Shimakawa for their efforts on human scanning and clinical application.References
1. Siu, A. L. & Force, U. S. P. S. T. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 164, 279-296, doi:10.7326/M15-2886 (2016).
2. von Euler-Chelpin, M., Lillholm, M., Vejborg, I., Nielsen, M. & Lynge, E. Sensitivity of screening mammography by density and texture: a cohort study from a population-based screening program in Denmark. Breast Cancer Res 21, 111, doi:10.1186/s13058-019-1203-3 (2019).
3. Carbonaro LA, Tannaphai P, Trimboli RM, et al. Contrast enhanced breast MRI: spatial displacement from prone to supine patient’s position. Preliminary results. Eur J Radiol. 2012;81:e771–e774. doi: 10.1016/j.ejrad.2012.02.013.
4. Satake H, Ishigaki S, Kitano M, et al. Prediction of prone-to-supine tumor displacement in the breast using patient position change: investigation with prone MRI and supine CT. Breast Cancer. 2016;23:149–158. doi: 10.1007/s12282-014-0545-z.
5. Arıbal E, Buğdaycı O. Supplementary abbreviated supine breast MRI following a standard prone breast MRI with single contrast administration: is it effective in detecting the initial contrast-enhancing lesions?. Diagn Interv Radiol. 2019;25(4):265-269. doi:10.5152/dir.2019.18167
6. Joukainen S, Masarwah A, Könönen M, Husso M, Sutela A, Kärjä V, Vanninen R, Sudah M. Feasibility of mapping breast cancer with supine breast MRI in patients scheduled for oncoplastic surgery. Eur Radiol. 2019 Mar;29(3):1435-1443. doi: 10.1007/s00330-018-5681-y. Epub 2018 Aug 17. PMID: 30120494.
7. Rossman P., et al., Characterization of a new ultra-flexible low-profile RF receive coil technology. Proceedings ISMRM 2017, 763.
8. Vasanawala S.S., et al., Development and Clinical implementation of very light weight and highly flexible Air technology arrays. Proceedings ISMRM 2017, 755.
9. Wake N, Ianniello C, Brown R, Walczyk J, Moy L, Collins C, Rusinek H. Design of a 3D Printed Patient-Specific Dual Compartment Breast Phantom. Proceedings of the ISMRM. May 11-16, 2019. Montreal, Canada.
Figures