1496
Static and dynamic functional connectivity in medication-free patients with obsessive compulsive disorder1Huaxi MR Research Center (HMRRC), Functional and molecular imaging Key Laboratory of Sichuan Province, Department of Radiology, West China Hospital, Sichuan University, Chengdu, China, 2Sichuan University, Chengdu, China
Synopsis
In current study, we use static and dynamic functional connectivity (sFC/dFC) to examine the connectivity alternation of bed nucleus of the stria terminalis (BNST) in medication-free patients with obsessive-compulsive disorder (OCD) to clarify the neural underpinnings of OCD. We found that BNST demonstrated different connected regions in sFC and dFC, indicating that the combination between sFC and dFC can help to detect BNST network alternations in OCD in a more comprehensive way by considering both the static and time-varying aspects.
Background
Obsessive-compulsive disorder (OCD), characterizing repetitive and persistent thoughts, images, impulses, and are commonly associated with anxiety 1. Emerging evidence suggests the bed nucleus of the stria terminalis (BNST) mediates anxiety through connections with other brain regions 2. Resting state functional connectivity (FC) is a common tool to identify the temporal correlations in spatially separated brain regions and is widely used for characterizing brain network alternations in mental disorders. Previous studies mostly assumed that the FC was constant during the magnetic resonance imaging (MRI) scanning. Recently, we have seen the emergence of interest in the temporal properties of FC (i.e., dynamic FC). However, there are no studies regarding dynamic FC (dFC) of the BNST in OCD patients. So in current study, we aimed to demonstrate whether OCD patients exist time-varying connectivity alternation using dFC and we also combine the traditional static FC (sFC) to help fully understand the characteristic change of BNST connectivity in OCD.Methods
A total of 87 medication-free OCD patients (age 29.06 ± 8.71) and 90 sex- and age- matched healthy controls (HC) (age 28.34 ± 10.85) were recruited in current study (Table 1). We used Yale-Brown Obsessive Compulsive Scale (Y-BOCS) to assess severity of OCD symptoms and used Hamilton Anxiety Scale (HAMA) and Hamilton Depression Scale (HAMD) to assess anxiety and depression level.All the subjects were scanned by a 3-Tesla GE MRI system. The T1 and resting state functional MRI images were obtained for each subject and preprocessed using DPARSF software (http://www.restfmri.net). The static and dynamic FC maps were estimated by DynamicBC toolbox (http://restfmri.net/forum/DynamicBC). The left and right BNST seed were generated using WFU PickAtlas 3.
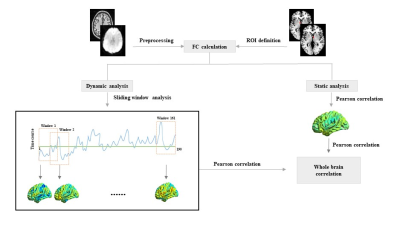
For sFC, we calculated the mean value during the whole session for each pair correlation. For dFC, we applied sliding window technique with a window size of 30 TRs (60 seconds) basing on the previous studies 4. The standard deviation (SD) maps of FC for each subject across 161 windows were calculated which were then used to assess the temporal variability of BNST-based functional connectivity. Then static maps and SD maps were standardized.
We used two-sample t-tests with false discovery rate correction (pcorr < 0.05 at the cluster level, puncorr < 0.001 at the voxel level) to demonstrate brain regions with significant differences between the two groups. In addition, to identify brain regions associate with clinical symptom severity, we performed whole brain correlation analysis using Pearson correlation. The procedures of present study were showed in Figure 1.
Results
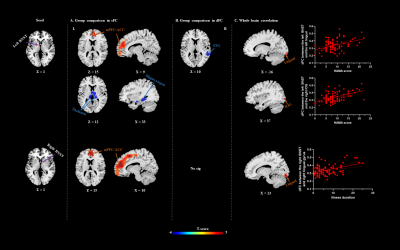
Static FC: We observed increased sFC between the left BNST and bilateral medial prefrontal cortex (mPFC) and anterior cingulate cortex (ACC), decreased sFC between the left BNST and right hippocampus and bilateral thalamus in OCD patients compared with HC. OCD patients also showed hyperconnectivity between the right BNST and the bilateral mPFC and ACC (Figure 2A and Table 2).Dynamic FC: Patients demonstrated decreased dFC between the left BNST and right superior temporal gyrus (STG) compared with HC. The dFC pattern of the right BNST did not significantly differ between groups (Figure 2B and Table 2).
Whole brain correlation: We found that the HAMA scores positively correlated with the dFC between the left BNST and the left lingual gyrus, between the left BNST and the right inferior occipital gyrus. In addition, there was also a positive correlation between the illness and the dFC between the right BNST and the right lingual gyrus (Figure 2C).
Discussion & Conclusion
In the present study, we investigated the static and dynamic connectivity alternations of BNST in medication-free patients with OCD for the first time. We observed that the connectivity patterns of BNST in sFC and dFC are completely different. Specifically, the BNST showed decreased sFC with regions involved emotion processing such as hippocampus and thalamus, and increased sFC with regions associated with cognitive control such as mPFC and ACC. On the other hand, the BNST revealed decreased time-varying connectivity to superior temporal gyrus related with sensory processing.Taken together, our results suggest the sFC and dFC provided different information and indicate their combination can help to detect abnormal connectivity pattern in a more comprehensive way by considering both the static and time-varying aspects. And this may be particular useful in mental disorders whose neural mechanism is still largely unknown.
Acknowledgements
This study was supported by National Nature Science Foundation (Grant NO. 81671669), Science and Technology Project of Sichuan Province (Grant NO. 2017JQ0001).References
1. Stein DJ, Costa DLC, Lochner C, et al. Obsessive-compulsive disorder. Nat Rev Dis Primers. 2019; 5(1): 52.
2. Avery SN, Clauss JA, Winder DG, et al. BNST neurocircuitry in humans. Neuroimage. 2014; 91: 311-23.
3. Rabellino D, Densmore M, Harricharan S, et al. Resting-state functional connectivity of the bed nucleus of the stria terminalis in post-traumatic stress disorder and its dissociative subtype. Hum Brain Mapp. 2018; 39(3): 1367-79.
4. Nalci A, Rao BD, Liu TT. Nuisance effects and the limitations of nuisance regression in dynamic functional connectivity fMRI. Neuroimage. 2019; 184: 1005-31.
Figures
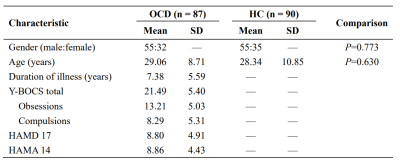
Table 1. Demographic and clinical characteristics of the participants. OCD, Obsessive-compulsive disorder; HC, Healthy Control; SD, standard deviation; Y-BOCS, Yale-Brown Obsessive-Compulsive Scale; HAMA, Hamilton Anxiety Scale; HAMD, Hamilton Depression Scale.
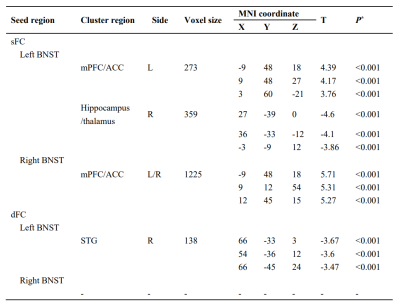
Table 2. Brain regions with significant differences in sFC and dFC between patients with OCD and HC. *P < 0.05 with whole-brain false discovery rate (FDR) correction at cluster level. sFC, static functional connectivity; dFC, dynamic functional connectivity; BNST, bed nucleus of the stria terminalis; mPFC, medial prefrontal cortex; ACC, anterior cingulate cortex; STG, superior temporal gyrus; L, left; R, right; MNI, Montreal Neurological Institute.