1491
The effect of white matter signal abnormalities on default mode network connectivity in mild cognitive impairment1PET/CT Unit, Medical Imaging, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China, 2Alzheimer's Clinical and Translational Research Unit, Department of Neurology, Massachusetts General Hospital, Charlestown, MA, United States, 3Athinoula A. Martinos Center for Biomedical Imaging, Department of Radiology, Massachusetts General Hospital, Charlestown, MA, United States, 4Medical Imaging, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China
Synopsis
The striking spatial overlap between regions of default mode network (DMN) and cortical areas most susceptible to Alzheimer's disease (AD)-related pathology and neurodegeneration, with alterations in DMN functional connectivity routinely observed among individuals with mild cognitive impairment (MCI). We examine the relative associations between white matter lesions of presumed vascular origin and cortical thinning typical of AD pathology with DMN integrity to elucidate mechanisms of disease. The degree of white matter damage may have a specific influence on precuneus and mPFC coupling and the observed preferential associations with white matter lesions support a vascular etiology to subtle impairment in MCI.
Manuscript
PurposeThe incidence of mild cognitive impairment (MCI) is common among older adults and often represents an early stage of Alzheimer’s disease (AD) neuropathology. Altered default mode network (DMN) functional connectivity has been reported in both MCI and AD, yet mechanisms underlying these differences are unclear. Regions within the DMN are particularly vulnerable to AD cortical pathology, but lesioned white matter within tracts connecting DMN cortical regions are also commonly observed. The purpose of this study is to investigate the differential effects of white matter lesion volume and neurodegenerative cortical atrophy on DMN functional connectivity in individuals with MCI.
Methods
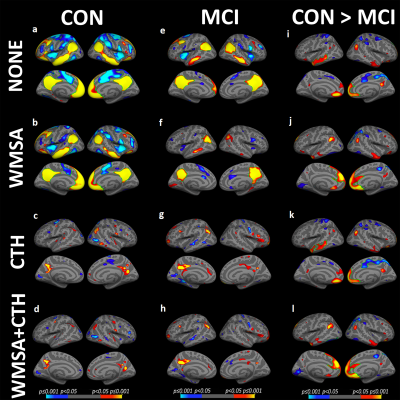
We examined associations between DMN seed-based connectivity, white matter signal abnormality (WMSA) load, and cortical atrophy in 17 individuals with neuropsychologically defined MCI, and 20 age, gender, and education-matched controls (CON). Enrolled participants were also administered comprehensive neuropsychological assessments. RESULTSMCI showed decreased functional connectivity (FC) between the precuneus-seed and bilateral lateral temporal cortex (LTC), medial prefrontal cortex (mPFC), posterior cingulate cortex, and inferior parietal lobe compared to those with controls. When controlling for white matter lesion volume, DMN connectivity differences between groups were diminished within bilateral LTC, although were significantly increased in the mPFC explained by significant regional associations between white matter lesion volume and DMN connectivity only in the MCI group. When controlling for cortical thickness, DMN FC was similarly decreased across both groups.
Results
MCI showed decreased functional connectivity (FC) between the precuneus-seed and bilateral lateral temporal cortex (LTC), medial prefrontal cortex (mPFC), posterior cingulate cortex, and inferior parietal lobe compared to those with controls. When controlling for white matter lesion volume, DMN connectivity differences between groups were diminished within bilateral LTC, although were significantly increased in the mPFC explained by significant regional associations between white matter lesion volume and DMN connectivity only in the MCI group. When controlling for cortical thickness, DMN FC was similarly decreased across both groups.
Discussion
The present study confirms prior findings of reduced functional connectivity in disparate regions of the DMN network in MCI relative to cognitively healthy controls [1-6], while extending this line of work to demonstrate that regional connectivity patterns differed both within and between groups as a function of WMSA volume and cortical thickness. Both structural measures differentially influenced group differences in functional connectivity between the precuneus-seed region and the LTC, IPL, and pCC, with WMSA exhibiting the strongest effect on DMN connectivity within mPFC regions.
Conclusion
These findings suggest that white matter lesions and cortical atrophy are differentially associated with alterations in FC patterns in MCI. Associations between white matter lesions and DMN connectivity in MCI further support at least a partial but important vascular contribution to age-associated neural and cognitive impairment.
Acknowledgements
This work is supported by the National Institutes of Health/NationalInstitute of Nursing Research R01 NR010827, National Natural Science Foundation of China under grant nos. 82001772, 81771914, 82071993, 81571752, 81571640 and Short-term PhD Mobility Program by Health ScienceCentre of Xi'an Jiaotong University.References
[1] Li Y, Wang X, Li Y, Sun Y, Sheng C, Li H, et al. Abnormal Resting-State Functional Connectivity Strength in Mild Cognitive Impairment and Its Conversion to Alzheimer's Disease. Neural Plast 2016;2016 4680972.
[2] Weiler M, Teixeira CV, Nogueira MH, de Campos BM, Damasceno BP, Cendes F, et al. Differences and the relationship in default mode network intrinsic activity and functional connectivity in mild Alzheimer's disease and amnestic mild cognitive impairment. Brain Connect 2014;4(8) 567-574.
[3] De Vogelaere F, Santens P, Achten E, Boon P, Vingerhoets G. Altered default-mode network activation in mild cognitive impairment compared with healthy aging. Neuroradiology 2012;54(11) 1195-1206.
[4] Chhatwal JP, Sperling RA. Functional MRI of mnemonic networks across the spectrum of normal aging, mild cognitive impairment, and Alzheimer's disease. J Alzheimers Dis 2012;31 Suppl 3 S155-167. [5] Bai F, Zhang Z, Yu H, Shi Y, Yuan Y, Zhu W, et al. Default-mode network activity distinguishes amnestic type mild cognitive impairment from healthy aging: a combined structural and resting-state functional MRI study. Neurosci Lett 2008;438(1) 111-115.
[6] Jin M, Pelak VS, Cordes D. Aberrant default mode network in subjects with amnestic mild cognitive impairment using resting-state functional MRI. Magn Reson Imaging 2012;30(1) 48-61.
Figures