1450
Initial Results of a Novel High-Resolution 3D-FSE Based Protocol for Silicone Breast Implant Screening1Division of Biomedical Physics, Food and Drug Administration, Silver Spring, MD, United States, 2Department of Radiology and Medical Imaging Research, University of Virginia, Charlottesville, VA, United States, 3Department of Radiology & Radiological Sciences, Uniformed Services University, Bethesda, MD, United States, 4Division of Imaging, Diagnostics, and Software Reliability, Food and Drug Administration, Silver Spring, MD, United States, 5Canon Medical Systems USA, Tustin, CA, United States
Synopsis
Conventional silicone breast MR involves multi-contrast 2D scans. However, the use of 2D imaging risks the loss of fine structure visualization in the 3rd dimension. An isotropic 3D-FSE pulse sequence was first tested in a single-center study in 13 subjects with silicone breast implants (SBI). The images were evaluated by radiologists for quality and added utility of the bilateral, 3D scans. To allow for multi-site implementation of the 3D sequence, a bilateral breast phantom containing lipid, fibroglandular mimic and a silicone implant was tested across major MR vendors to ensure adequate signal-to-noise ratios and tissue contrast.
Introduction
The U.S. FDA recommends that women with silicone breast implants (SBI) get regular screenings for rupture1. Current clinical MRI protocols use 2D multi-slice techniques, with combinations of inversion-recovery based silicone, fat or water suppression. Imaging is performed in multiple planes, unilateral or bilateral, with typical procedures lasting approximately 30 to 45 minutes. Although the inherent signal-to-noise ratio (SNR) is excellent with modern MRI hardware, there is still an unacceptable level of false positive findings2,3. We hypothesize that the main mechanism of false positive outcome is the use of a thick slice (3-4 mm) for 2D imaging, which can obscure and confound detection of the signal from intricate folds in the silicone pouch. The objective of this work was to develop a standardized 3D-FSE protocol for routine clinical application across common MRI platforms. Our approach was to keep the level of complexity low to allow implementations across a variety of vendors/scanner models, by simple modification of existing 3D FSE protocols provided by the vendor.Methods
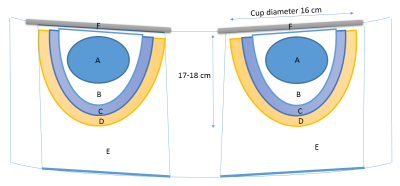
A novel 3D protocol, based on an available 3D-FSE pulse sequence, was first tested in a single-center study in 13 subjects with SBIs. The center’s 2D SBI imaging protocol was performed (~30 minutes) followed by the novel 3D protocol (~5 min). The images were evaluated by radiologists for quality, diagnostic confidence, and added utility of the bilateral, 3D scans. To allow for implementation of the 3D sequence/protocol across vendors, a bilateral breast phantom containing lipid, fibroglandular mimic and a silicone implant was developed (Figure 1). The 3D sequence (mean TR/TE: 1031/182ms and voxel size 1x1x1mm3) was implemented on MR systems from major vendors (4 at 1.5T, 3 at 3.0T). Segmentation to determine the silicone, fibroglandular, saline, and lipid regions was completed manually using 3DSlicer (Kitware). Silicone signal-to-noise ratios (SNR) were determined using the difference-of-images method4. In addition to silicone SNRs, the silicone signal was compared to the lipid and fibroglandular signals to assess tissue contrast.Results
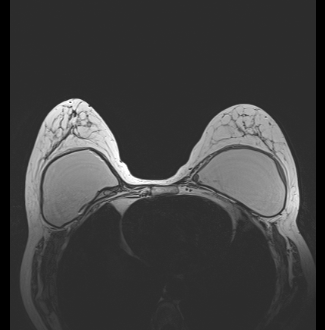
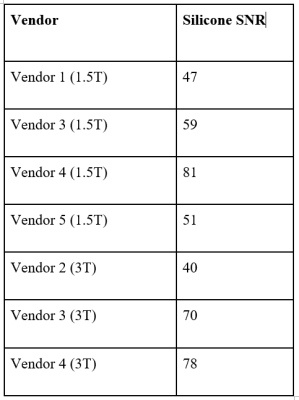
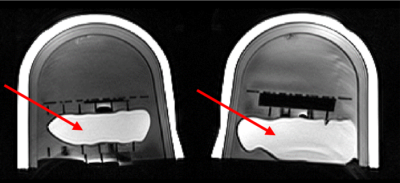
3D-FSE images were acquired successfully for all 13 patients, and image quality for 8 subjects was found to be satisfactory. Motion artifacts and incorrectly placed center frequencies accounted for the 5 unsatisfactory patient images. The pilot study SNRs had an average value of 36 ± 14. A sample scan from a patient with an intact silicone implant is shown in Figure 2, which shows excellent delineation of the wall of the silicone implant. The mean silicone SNR in the phantom was found to be 59 ± 13 and 63 ± 16 for 1.5T and 3.0T systems, respectively. The SNR values for each vendor are visible in Figure 3 and a sample scan of the breast phantom is provided in Figure 4. The average value of the lipid-silicone ratio was 3.1 ± 1.3 and the fibroglandular-silicone ratio was 1.7 ± 1.2.Discussion
The breast phantom with components for lipid, fibroglandular tissue and silicone provided a viable approach to standardize a 3D protocol across different vendors. The novel 3D-FSE protocol was generated using existing 3D T2-weighted protocols and hence can be implemented over a broad user base. The breast phantom silicone SNR results showed variability between scanners; however, they exceeded the SNRs achieved during the pilot study in all cases but one. Additionally, the 1mm isotropic spatial resolution allowed resolution of the 2-cm grid placed inside the phantom, as well as intricate folds of the implant. The lipid signal was consistently higher than the silicone signal, and the fibroglandular signal was on average higher than the silicone signal but significantly more variable. High contrast between the lipid and fibroglandular tissues and the silicone can be useful to obtain an accurate diagnosis of SBI rupture because it provides clear distinction in the case of silicone leakage. However, in most cases, the detection of SBI rupture, as well as intricate confounding folds, will be aided by well-defined edges of the implant.Conclusion
The diagnostic results from the pilot study and the comparable SNR values from the multi-site phantom scans indicate that our 3D MRI breast implant screening protocol is ready for clinical translation.Acknowledgements
DISCLAIMER: The mention of commercial products, their sources, or their use in connection with material reported herein is not to be construed as either an actual or implied endorsement of such products by the Department of Health and Human ServicesReferences
1. Center for Devices and Radiological Health: Update on the Safety of Silicone Gel-Filled Breast Implants (2011) - Executive Summary, FDA.
2. Benedetto GD, Cecchini S, Grassetti L, et al.: Comparative Study of Breast Implant Rupture Using Mammography, Sonography, and Magnetic Resonance Imaging: Correlation with Surgical Findings. The Breast Journal 2008; 14:532–537.
3. Lindenblatt N, El-Rabadi K, Helbich TH, Czembirek H, Deutinger M, Benditte-Klepetko H: Correlation between MRI results and intraoperative findings in patients with silicone breast implants. Int J Womens Health 2014; 6:703–709.
4. Dietrich O, Raya JG, Reeder SB, Reiser MF, Schoenberg SO: Measurement of signal-to-noise ratios in MR images: Influence of multichannel coils, parallel imaging, and reconstruction filters. Journal of Magnetic Resonance Imaging 2007; 26:375–385.
Figures