1427
SNR of Flexible Versus Rigid Coil Arrays for Knee MRI1Department of Bioengineering, Stanford University, Stanford, CA, United States, 2Department of Radiology, Stanford University, Stanford, CA, United States, 3Department of Electrical Engineering, Stanford University, Stanford, CA, United States
Synopsis
Flexible extremity coil-arrays for knee imaging in MRI can improve coil positioning and comfort to patients in the scanner and wrap tightly around the knee, placing coil elements close to anatomy of interest. Despite this, flex coils have not been widely adapted due to perceived superiority of the SNR of transmit-receive coils. In this study, we analyzed the SNR of flex coil-arrays versus a rigid coil-array in phantom and in vivo to determine which coil-arrays had improved SNR. Preliminary results suggest that flexible coil-arrays show comparable or increased SNR and generally more uniform SNR over rigid coil-arrays.
Introduction
MRI is commonly used in the clinic for knee evaluation and diagnosis, with around 1.25 million clinical knee scans performed annually in the US.1 Standard clinical knee imaging protocols for MRI call for dedicated transmit and receive (T/R) knee coils to improve the image quality for knee evaluation.2 Alternatively, flex coils in MRI can improve coil positioning and comfort to patients in the scanner and allow for coil elements to be placed closer to the anatomy of interest. Furthermore, such coil-arrays also incorporate more elements, potentially allowing better conditioning of g-factor maps for parallel imaging. However, these flexible coils have not been widely adopted due to the perceived superiority of T/R coils for extremity imaging.In this study, we compared pixel-wise SNR maps using a GRAPPA-based image reconstruction and pseudo multiple replica approach3 for a state-of-the-art dedicated hard-shell T/R knee coil and flexible extremity coil-arrays, in both phantoms and healthy human subjects.
Methods
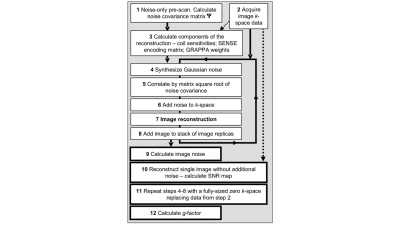
Images were acquired on a 3.0T scanner (GE Healthcare, Milwaukee, WI, USA) using a quantitative double-echo in steady-state sequence (qDESS). A single large cylindrical phantom, a phantom consisting of 6 fluid-filled falcon tubes, and the right knee of two healthy subjects were imaged to assess SNR. Phantoms were scanned using 3 coils: a medium 16-channel receive-only flexible extremity coil (NeoCoil, Pewaukee, WI, USA), a large 16-channel receive-only flexible extremity coil (NeoCoil, Pewaukee, WI, USA), and a rigid 18-channel transmit-receive dedicated knee coil (Quality Electrodynamics, Cleveland, OH). Two human subjects were scanned with the medium flex coil and rigid coil. Image reconstruction for both datasets were performed in the GE Orchestra framework using complex coil combination, with the in vivo dataset employing ARC reconstruction.We utilized a Monte Carlo-based, pseudo-multiple replica approach outlined in Robson et al.3 for 200 repetitions to calculate SNR maps for both coil arrays (Figure 1). This method uses a multi-channel noise covariance matrix from the scans to estimate the correlated Gaussian noise present in the k-space data. For each repetition, a random sample of this noise is added to the acquired k-space data and reconstructed. A standard deviation is calculated between all replicated images to estimate pixel-wise noise standard deviations, and the SNR is estimated using the acquired k-space data as the signal.
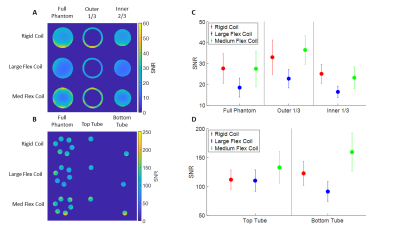
For the phantom dataset, average SNR was calculated in the cylindrical phantom and 6-tube phantom. Masks were used to isolate the outer third of the cylindrical phantom from the inner portion to investigate the average SNR differences at the surface and the interior of the phantom. For the 6-tube phantom, masking was done to isolate the top tube and the bottom tube in the phantom to compare average SNR differences between opposite regions on the surface of the phantom.
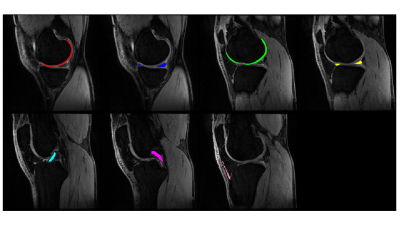
For the in vivo datasets, single-slice regions of interest were segmented: central slices for lateral femoral cartilage, medial femoral cartilage, lateral meniscus, and medial meniscus, and single slices for ACL, PCL, and patellar tendon (Figure 2). Data was analyzed by comparing the mean and standard deviation of the tissue SNR across coils and subjects.
Results
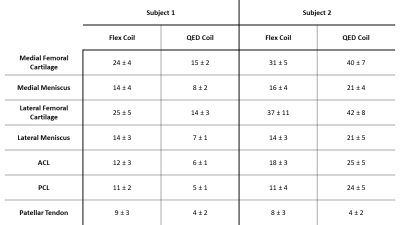
The processed SNR maps for the phantom datasets are shown in Figure 3, with central slices shown for each phantom and coil. Of note, the medium flex coil appears to have slightly better SNR on the outer third of the cylindrical phantom, reinforced by the mean SNR results shown in Figure 3c-d. The rigid coil only has comparably high SNR at the bottom region of the cylindrical phantom. In the 6-tube phantom, the medium flex coil had higher SNR in both the top and bottom tubes compared to the rigid and large flex coils.The SNR averages computed from the tissue segmented in vivo are shown in Figure 4. Of note, the two subjects seemed to differ in which coil had overall better SNR performance. For the first subject, the flex coil performed the best for every tissue analyzed, but for the second subject, the rigid coil performed the best, except in the patellar tendon.
Discussion
We examined the effect of rigid and flex coils on SNR in phantoms and knees in vivo. First, looking at the phantom data, the SNR at the surfaces of the phantoms is more uniform when imaged with the medium flex coil, as well as notably improving SNR at the surface compared to the rigid coil. This overall improvement in surface SNR is most likely due to the flex coil wrapped tightly around the phantom, as opposed to the rigid coil where the phantom sits on the bottom surface of the coil.In the in vivo data, the differences in SNR between the two coils appear to differ between subjects. One external factor that could explain this would be subject size differences, potentially causing the substantial variations in SNR seen here. Notably, the SNR of the patellar tendon was higher for the flex coil in both subjects, which is probably due to the ability to wrap the flex coil tightly on the anterior side of the knee.
Conclusion
Preliminary phantom and in vivo knee data suggest that flexible coil-arrays show comparable or increased SNR and generally more uniform SNR over rigid coil-arrays.Acknowledgements
Research support provided by NIH R01-AR077604, NIH K24-AR062068, PHIND Seed Grant, and GE Healthcare.References
1. Chaudhari A, Stevens K, Sveinsson B, Wood J, Beaulieu C, Oei E.H., Rosenberg J, Kogan F, Alley M, Gold G, and Hargreaves B. Combined 5-Minute Double-Echo in Steady-State with Separated Echoes and 2-Minute Proton-Density-Weighted 2D FSE Sequence for Comprehensive Whole-Joint Knee MRI Assessment. Journal of Magnetic Resonance Imaging. (2019), 49(7), e183-e194.
2. Bolog, N.V., Andreisek, G. Reporting knee meniscal tears: technical aspects, typical pitfalls and how to avoid them. Insights Imaging 7, 385–398 (2016).
3. Robson PM, Grant AK, Madhuranthakam AJ, Lattanzi R, Sodickson DK, McKenzie CA. Comprehensive quantification of signal-to-noise ratio and g-factor for image-based and k-space-based parallel imaging reconstructions. Magn Reson Med. 2008;60(4):895-907.
Figures