1384
Motion-robust T2-weighted TSE imaging in the prostate by performing non-rigid registration between averages1Institute of Radiology, Martha-Maria Hospital, Nuremberg, Germany, 2MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
The major reason for artifacts in T2-weighted prostate imaging is motion-induced blurring caused by slight displacements between averages. Here, a non-rigid elastic registration is proposed to properly align the images before averaging. The method is evaluated in 12 patients and is shown to improve image quality in 71% of all investigated cases. Identification of pathology was improved in 42%. While only 58% of the conventional images achieved good or excellent image quality, this was the case for 88% when applying motion correction. As demonstrated, non-rigid registration results in clearly reduced motion artifacts and improves image quality and diagnostic confidence.
Introduction
T2-weighted imaging has high relevance in multi-parametric prostate MRI, especially for the transition zone1. The major reason for artifacts is motion-induced blurring, which can lead to non-diagnostic scans and costly follow-up examinations.The current solution comprises laxative measures before examination and usage of bowel relaxants. However, these cannot be applied to all patients (contraindications like glaucoma, patient unfit to drive) and require more complex patient handling (administration of relaxants). Furthermore, residual motion and corresponding artifacts can even occur with bowel relaxants 2. The aim of this work is to implement motion-robust T2-weighted prostate imaging and to evaluate image quality and identification of suspected tumor areas.
Methods
T2-weighted Turbo Spin-Echo (TSE) for prostate imaging is clinically acquired with several averages to yield sufficient SNR for reliable diagnosis. Potential sources of reduced image quality and blurring are bowel motion caused by peristalsis and slight movement of the caudal abdominal wall. Since bowel motion is known to occur typically in intervals with alternating phases of relative tranquilly and motility, it appears plausible that individual averages (with an acquisition time of about one minute) usually do not show motion-related artifacts. As movement leads to slight displacements between different averages, the averaged image, however, may show blurring and reduced delineation of small structures (figure 1). Hence, we propose a non-rigid elastic registration before averaging to properly align the images. In detail, a dense deformation field is computed on three subsequent resolution levels using local cross-correlation as similarity measure 3.For clinical evaluation, 12 consecutive prostate patients were scanned on a 3T scanner (MAGNETOM Vida, Siemens Healthcare, Erlangen, Germany) with a bi-parametric MRI program (T2-weighted and diffusion-weighted imaging) without administration of bowl relaxant. All patients were suspected of prostate cancer by elevated prostate-specific antigen, suspicious digital-rectal examination or positive family history and gave written informed consent before examination.
For T2-weighted imaging, a prototypical TSE sequence was applied in axial and coronal orientation (TE/TR 104/7500 ms, typical TA 3:15 min, spatial resolution 0.3(i) x 0.3(i) x 3.0 mm3, 3 averages). Final images were reconstructed with both the product implementation (without motion correction (MOCO)) and the described MOCO which was integrated in the scanner reconstruction pipeline.
For all patients, axial and coronal images were evaluated, resulting in 24 image series. Reading was performed by two experienced radiologists (>20 years / >10 years of experience in prostate MRI, respectively) in consensus. Image quality (contrast and resolution) and identification of suspect areas (PI-RADS ≥3) were rated applying a 4-point Likert-scale. A score of 1 means excellent contrast and resolution and pathology is clearly visible, while a score of 4 means poor image quality and pathology is not visible (table 1).
Results
In 71% of all image series, image quality of MOCO was rated as better than the conventional reconstruction (table 2, figure 2). Within these, the score increased by 1 point in 71%, and by two points in 29%. In the remaining 29% of all image series, both the conventional and the MOCO reconstruction achieved similar quality. Here, the conventional reconstruction already achieved excellent quality (Likert-score of 1) in 86%. Only in one series, the Likert-score of 3 could not be improved.Six patients achieved a PI-RADS score ≥3. Here, the identification of the suspect area was improved in 42 % of the image series (figure 3).
Discussion
In our feasibility study, the proposed MOCO outperformed the conventional reconstruction with respect to image quality and identification of suspect areas. As expected, image quality remains constant when applying the proposed motion correction for cases where no motion was present. 88% of the MOCO images resulted in good or excellent image quality, whereas only 58% of the conventional images achieved a similar score. The identification of tumor suspect areas was good or excellent in all cases applying MOCO. Nevertheless, the proposed registration cannot address motion occurring on a shorter time scale such as e.g. breathing motion. This might be the reason that image quality of 13% of the series was still rated as fair, also after applying the MOCO.Prostate motion during examination is usually caused by rectal or patient movement. In prior studies, the negative effect of rectal distension2 and the benefit of bowel relaxants to reduce rectal movements4 were demonstrated.
In our study, examinations were performed without bowel relaxant. In 42% of all cases motion caused degraded image quality (Likert-score 3 or 4), 70% of them could be improved to a score of 1 or 2 by the MOCO. To answer the question whether the proposed technique allows omitting bowel preparation, image quality of the conventional technique with bowel relaxant should be compared to the MOCO without bowel relaxant. Furthermore, the preliminary results of 12 patients presented here require confirmation in a bigger cohort, which is ongoing work.
Conclusion
Although being a rather simple technique, the proposed non-rigid registration results in clearly reduced motion artifacts and therefore can improve image quality and increase diagnostic confidence. In consequence, it enables motion-robust T2-weighted prostate imaging while potentially overcoming the need for bowel relaxants and follow-up examinations.Acknowledgements
No acknowledgement found.References
1. Turkbey B, Rosenkrantz AB, Haider MA et al. (2019) Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol 76: 340–351. https://doi.org/10.1016/j.eururo.2019.02.033
2. Padhani AR, Khoo VS, Suckling J et al. (1999) Evaluating the effect of rectal distension and rectal movement on prostate gland position using cine MRI. Int J Radiat Oncol Biol Phys 44: 525–533. https://doi.org/10.1016/s0360-3016(99)00040-1
3. Jolly MP, Guetter C, Guehring J (2010) Cardiac segmentation in MR cine data using inverse consistent deformable registration: IEEE ISBI 2010
4. Caglic I, Hansen NL, Slough RA et al. (2017) Evaluating the effect of rectal distension on prostate multiparametric MRI image quality. Eur J Radiol 90: 174–180. https://doi.org/10.1016/j.ejrad.2017.02.029
Figures
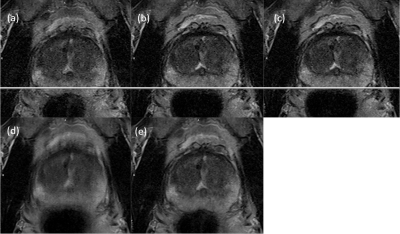
Figure 1: Typical
motion in T2-weighted imaging with averaging
(a-c) single average with degraded image quality and displacement shift
(d) combination of all averages without MOCO
(e) combination of all averages with MOCO and improved image quality
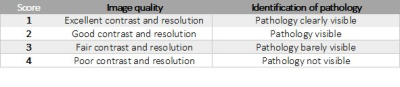
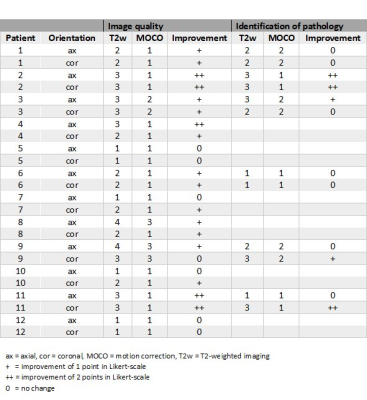
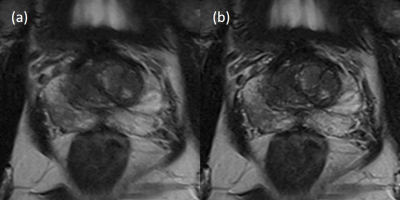
Figure 2: Improved
image quality of MOCO
(a) conventional reconstruction
(Likert-score 3)
(b) MOCO (Likert-score
1)
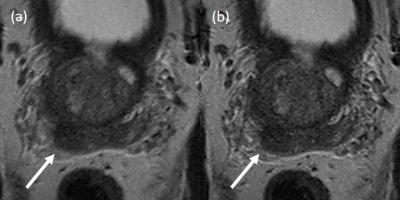
Figure 3: Improved
identification of pathology (PI-RADS 3 lesion)
(a) conventional
reconstruction (Likert-score 3)
(b) MOCO (Likert-score
1)