1351
Diffusion-Weighted Imaging with Integrated Slice-Specific Dynamic-Shimming for Rectal Cancer Detection and Characterization1Peking University First Hospital, Beijing, China, 2MR Collaboration, Siemens Healthcare Ltd China, Beijing, China, 3MR Application Development, Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
Diffusion-weighted imaging (DWI) with integrated slice-specific dynamic-shimming (iShim) could improve image quality compared with conventional 3D-Shimming single-shot echo-planar-imaging (SS-EPI) DWI in patients with rectal cancer. iShim DWI can help differentiate rectal cancer from normal walls and predict pathologic characterizations. iShim DWI could be an effective and promising approach and a good alternative to conventional 3D-Shimming SS-EPI DWI for patients with rectal cancer.
Background and Purpose
In recent years, single-shot echo-planar-imaging (SS-EPI) diffusion-weighted imaging (DWI) has been widely used in bladder, prostate, breast, and thyroid cancers. But its known geometric distortion and T2* blurring have limited DWI applications in rectal cancer imaging. Recently, iShim-DWI was introduced to improve image quality and lesion detection. This study aimed to compare iShim-DWI with conventional 3D-Shimming SS-EPI DWI looking at image quality and the pathologic characterizations of rectal cancer.Materials and Methods
One hundred and ninety-three consecutive patients with rectal tumors were enrolled for a retrospective analysis. Among these patients, 101 underwent prototype iShim DWI (b=0, 800, and 1600 s/mm2), and 92 underwent conventional 3D-Shimming SS-EPI DWI (b=0 and 1000 s/mm2) on a 1.5T MR system (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany) with an 18-channel body coil and a 32-channel spine coil.Qualitative analysis of the DWI images was performed by two independent readers, including assessments of adequate fat suppression, the presence of image artifacts, and image quality. The assessments were performed in a Likert-type manner:1) Adequate fat suppression in the DWI images. Score 1: fat suppression failure Score 2: regional fat-water failure but still interpretable Score 3: minimal failures at the image periphery Score 4: perfect fat-water separation2) The presence of artifacts on both the DWI images and ADC maps. Score 1: non-diagnostic Score 2: artifacts but diagnostic Score 3: no artifacts 3) Image quality for both the DWI images and ADC maps: Score 1: non-diagnostic image quality with serious artifacts, image distortion, or poor signal intensities Score 2: poor diagnostic image quality and reader diagnostic confidence, with serious artifacts, pronounced image distortions, or relatively poor signal intensities Score 3: moderate image quality and reader confidence with some artifacts and moderate image distortionsScore 4: good diagnostic image quality and reader confidence with few artifacts, slight image distortions, and well-delineated anatomic structures (e.g., rectal wall) Score 5: excellent image quality and strong reader confidence in diagnosing rectal cancer with almost no artifacts or imaging distortionsQuantitative analyses were performed by calculating standard deviations (SDs) of the gluteus maximus, signal intensities (SIs) of the lesion and residual normal rectal wall tissue, apparent diffusion coefficient (ADC) values, and image quality parameters, such as signal-to-noise ratios (SNRs) and contrast-to-noise ratios (CNRs) of primary rectal tumors. For patients with primary rectal cancer, two pathologic groups were formed according to the pathologic results: Group 1 (well-differentiated) and Group 2 (poorly differentiated). Statistical analyses were performed with a p <0.05 considered significantly different.
Results
Compared with conventional 3D-Shimming SS-EPI DWI, significantly higher scores of image quality were obtained in iShim DWI images (P<0.001). The SDbackground was significantly reduced in b1600 images and ADC maps of iShim DWI. Both SNR and CNR of b=800 s/mm2 and b=1600 s/mm2 images in iShim DWI were higher than that of b=1000 s/mm2 images in conventional 3D-Shimming SS-EPI DWI. In primary rectal cancer of the iShim cohort, SIlesion was significantly higher than SIrectum in both b=800 s/mm2 and b=1600 s/mm2 images. ADC values were significantly lower in Group 2 (732±85) mm2/s) than that in Group 1 ((912±207) mm2/s). ROC analyses showed the significance of ADC and SIlesion values between the two groups.Conclusion
DWI of iShim with b values of 800 and 1600 s/mm2 is a promising rectal tumor imaging technique and has the potential ability to differentiate rectal cancer from normal wall architecture and predict pathologic characterizations in rectal cancer patients.Acknowledgements
No acknowledgement found.References
[1] Gatidis S, Graf H, Weiß J, Stemmer A, Kiefer B, Nikolaou K, Notohamiprodjo M, Martirosian P. Diffusionweighted echo planar MR imaging of the neck at 3 T using integrated shimming: comparison of MR sequence techniques for reducing artifacts caused by magnetic-field inhomogeneities. MAGMA. 2017; 30:57–63.[2] Zhang H, Xue H, Alto S, Hui L, Kannengiesser S, Berthold K, Jin Z. Integrated Shimming Improves Lesion Detection in Whole-Body Diffusion-Weighted Examinations of Patients With Plasma Disorder at 3 T. Invest Radiol. 2016; 51:297–305.[3] Chen L, Sun P, Hao Q, Yin W, Xu B, Ma C, Stemmer A, Fu C, Wang M, Lu J. Diffusion-weighted MRI in the evaluation of the thyroid nodule: Comparison between integrated-shimming EPI and conventional 3D-shimming EPI techniques. Oncotarget 2018;9(40):26209-26216. doi:10.18632/oncotarget.25279.[4] Li H, Liu L, Shi Q, Stemmer A, Zeng H, Li Y, Zhang M. Bladder cancer: detection and image quality compared among iShim, RESOLVE, and ss-EPI diffusion-weighted MR imaging with high b value at 3.0 T MRI. Medicine (Baltimore) 2017;96(50):e9292. doi:10.1097/MD.0000000000009292.[5] Gatidis S, Graf H, Weiß J, Alto Stemmer A, Kiefer B, Nikolaou K, Notohamiprodjo M, Martirosian P. Diffusion-weighted echo planar MR imaging of the neck at 3 T using integrated shimming: comparison of MR sequence techniques for reducing artifacts caused by magnetic-field inhomogeneities. MAGMA 2017;30(1):57–63. doi: 10.1007/s10334-016-0582-z.[6] Lee SK, Tan ET, Govenkar A, Hancu I. Dynamic slice-dependent shim and center frequency update in 3 T breast diffusion weighted imaging. Magn Reson Med 2014;71(5):1813–1818. doi: 10.1002/mrm.24824.[7] Naranjo ID, Gullo RL, Morris EA, Larowin T, Fung MM, Guidon A, Pinker K, Thakur SB. High-Spatial-Resolution Multishot Multiplexed Sensitivity- encoding Diffusion-weighted Imaging for Improved Quality of Breast Images and Differentiation of Breast Lesions: A Feasibility Study. Radiology 2020; 2(3):e190076. doi:10.1148/rycan.2020190076.[8] Zhang H, Xue H, Alto S, Hui L, Kannengiesser S, Berthold K, Jin Z. Integrated shimming improves lesion detection in whole-body diffusion-weighted examinations of patients with plasma disorder at 3 T. Invest Radiol 2016;51:297–305. doi: 10.1097/RLI.0000000000000238.Figures
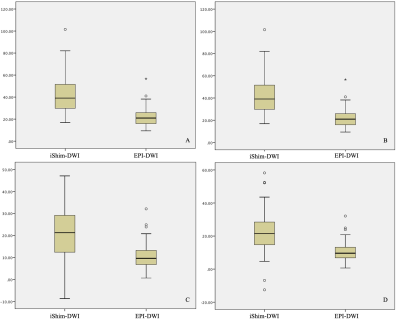
Figure 1. Boxplots of SNR and CNR ratios of primary rectal tumors between iShim-DWI andSS-EPI DWI.
A: SNR of primary rectal tumor in b800 of iShim-DWI shown significantly high compared to b1000 of EPI-DWI (P<0.001).B: SNR of primary rectal tumor in b1600 of iShim-DWI shown significantly high compared to b1000 of EPI-DWI (P<0.001).C: CNR of primary rectal tumor in b800 of iShim-DWI shown significantly high compared to b1000 of EPI-DWI (P<0.001).D: CNR of primary rectal tumor in b1600 of iShim-DWI shown significantly high compared to b1000 of EPI-DWI (P<0.001).
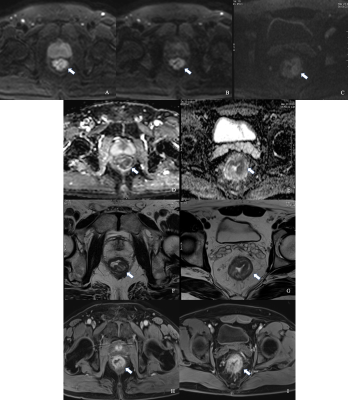
Figure 2 Comparison between iShim- and SS-EPI-DWI in patients after CRT.
Images on the left side were on the same location in patients with iShim-DWI. Images on the right side were on the same location in patients with SS-EPI-DWI. iShim-DWI of b800 (A) and b1600 (B) showed higher SNR and CNR with lower signal noise compared with SS-EPI-DWI of b1000 (C). ADC map (E) of iShim-DWI showed better image quality compared with ADC map (F) of SS-EPI-DWI. T2W images (F and G) and dynamic T1W images (H and I) showed the same location of lesion (arrows) for iShim- and SS-EPI- cohort, respectively.
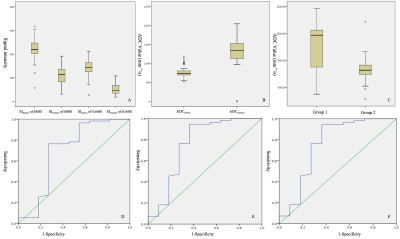
Figure 3 Boxplot of Quantitative Assessment of primary rectal cancer in iShim-DWI
A: Signal intensity (SI) shown significantly high in primary rectal cancer compared to residual rectal wall in iShim.B: ADC values shown significantly low in primary rectal cancer compared to residual rectal wall in iShim.C: ADC values comparison shown difference between two pathological groups (Group 1: well differentiated and Group 2: moderate to lower differentiated) D-F: ROC analysis between two groups shown significance in SI-lesion of b800, SI-lesion of b1600 and ADC maps, respectively.
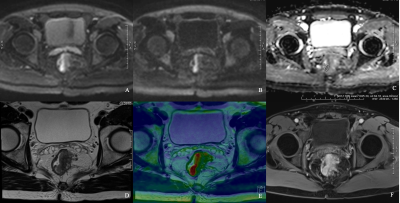
Figure 4 iShim DWI for patient with primary rectal cancer of Grade 1
DW images of b800 (A), b1600 (B), ADC map (C), T2WI (D), infusion images of both T2WI and DWI (E) and dynamic T1WI (F) showed the same location of lesion. Average ADC value measured was 1025.39 mm2/s (C).
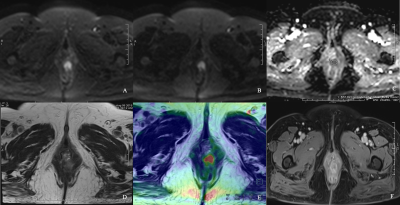
Figure 5 IShim DWI for patient with primary rectal cancer of Grade 3
DW images of b800 (A), b1600 (B), ADC map (C), T2WI (D), infusion images of both T2WI and DWI (E) and dynamic T1WI (F) showed the same location of lesion. Average ADC value measured was 723.27 mm2/s (C).