1301
Correlating Concussion-Related Symptoms to the Personalized MRI Assessment of Brain Abnormalities in Children1School of Biomedical Engineering, McMaster University, Hamilton, ON, Canada, 2Imaging Research Centre, St. Joseph's Healthcare Hamilton, Hamilton, ON, Canada, 3School of Rehabilitation Sciences, McMaster University, Hamilton, ON, Canada, 4Department of Psychology, Neuroscience & Behaviour, McMaster University, Hamilton, ON, Canada, 5ARiEAL Research Centre, McMaster University, Hamilton, ON, Canada, 6Department of Linguistics, McMaster University, Hamilton, ON, Canada, 7Department of Electrical and Computer Engineering, McMaster University, Hamilton, ON, Canada, 8Department of Radiology, McMaster University, Hamilton, ON, Canada
Synopsis
Although concussion diagnosis is often subjective, DTI can effectively quantify brain white matter damage. In this study, demographic and DTI metrics were compared between 26 paediatric concussion subjects against 49 healthy age and sex matched controls. FA was significantly reduced in injured brain regions and correlated with younger age and worsened symptoms. RD was significantly increased in injured brain regions and correlated with younger age and the interaction between time to scan and PCSS score. Based on these results, age affects concussion severity in younger children resulting in worse symptoms and a greater number of abnormal brain regions.
Introduction
A quantitative diagnostic tool is required to effectively understand concussion-related symptoms, brain damage and recovery. Diffusion tensor imaging (DTI) can accurately characterize changes in white matter (WM) integrity following a concussion by measuring voxel-wise water diffusion metrics such as fractional anisotropy (FA), axial diffusivity (AD) and radial diffusivity (RD).1 After sustaining a concussion, children are more likely to suffer from worsened symptoms and a longer recovery than adults.2 However, the comparison of clinical demographic information against MRI data has often been overlooked in concussion-based MRI research. The purpose of this research was to determine if DTI metrics were correlated with clinical demographic information in paediatric concussion subjects. It was hypothesized that greater WM injury, measured by total injury burden, would correlate with worsened symptoms in younger subjects.Methods
Paediatric concussion subjects (n=26, 9 male/17 female, mean age 14.22 ± 2.64) were recruited from the Emergency Department of the McMaster Children’s Hospital following a recent concussion. Healthy age and sex matched control data (n=49) was downloaded from the NIH MRI Study of Normal Brain Development.3 For concussion subjects, demographic information was collected such as age at the time of injury, time between injury and MRI scan, and Post-Concussion Symptom Scale (PCSS) 4 score. Concussion subjects were scanned using a 3T GE Discovery MR750 MRI system and a 32-channel head and neck coil (General Electric Healthcare, Milwaukee, WI). Patient-specific brain injuries were identified and quantified against healthy, normative values using a statistical Z-scoring approach. Processing of all MRI data was performed using FSL, 5 where subject-specific Z-scoring was determined using MATLAB (v. R2020b). The correlation of injury burden with concussion symptoms and subject demographics was completed using multiple linear regression implemented in R (v.3.6.1) and RStudio (v.1.2.1335).Results
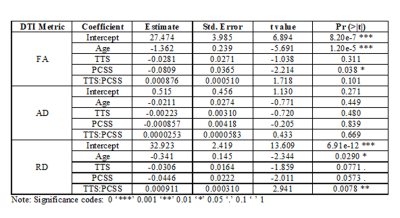
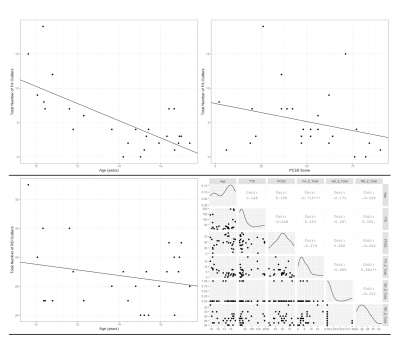
Demographic features were significantly correlated with total injury burden, defined as the total number of brain ROIs with outlier Z-scores per DTI metric per subject, of FA (Adjusted R-squared: 0.5725, p<0.001) and RD (Adjusted R-squared: 0.3295, p=0.013) (Table 1). Significantly reduced FA was positively associated with age at injury (p<0.001) and increased symptom severity indicated by PCSS score (p=0.038) (Figure 1). Further, significantly increased RD was correlated with age at injury (p=0.029) and the interaction between time to scan and PCSS score (p=0.0078) (Figure 1). There were no significant correlations between AD and demographic data.Discussion
Personalizing concussion assessment using DTI metrics successfully quantified the total injury burden based on abnormalities of specific brain ROIs. The results supported the hypothesis that a loss of WM integrity would correlate with injury related demographic information. Furthermore, the results also confirmed that PCSS and DTI are effective diagnostic tools for paediatric concussion. The correlation statistics indicated that age influenced injury severity, as seen by increased injury burden in younger subjects, and that worsened concussion symptoms aligned with a greater injury burden. It was proposed that these results occurred due to ongoing neurodevelopment in paediatric brains.Conclusion
Further research is required to include a greater number of paediatric subjects to corroborate these results. Moreover, other diffusion MRI techniques, such as HARDI or DKI, could be used to more accurately model the structure and integrity of WM. However, based on the findings of this research it is suggested that age must be considered for the diagnosis and treatment of concussions.Acknowledgements
No acknowledgement found.References
[1] Asken BM, DeKosky ST, Clugston JR, et al. Diffusion tensor imaging (DTI) findings in adult civilian, military, and sport-related mild traumatic brain injury (mTBI): a systematic critical review. Brain Imaging and Behav. 2018;12(2):585–612.
[2] Zuckerman S, Lee Y, Odom M, et al. Recovery from sports-related concussion: days to return to neurocognitive baseline in adolescents versus young adults. Surg Neurol Int. 2012;3(1):130.
[3] Rivkin M, Ball W, Wang D, et al. NIH: National Database for Autism Research - Paediatric MRI. http://paediatricmri.nih.gov. Accessed May 5, 2016.
[4] Lovell MR, Iverson GL, Collins MW, et al. Measurement of symptoms following sports-related concussion: reliability and normative data for the Post-Concussion Scale measurement of symptoms following sports-related concussion: reliability and normative data for the Post-Concussion Scale. Appl Neuropsychol. 2006;13(3):166–174.
[5] Jenkinson M, Beckmann C, Behrens T, et al. FSL. Neuroimage. 2012;62:782–790.
Figures