1130
Quantitative evaluation of different models of diffusion-weighted MRI for the correlation with molecular subtype of breast cancer1Radiology, Provincial Clinical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou, China, 2Provincial Clinical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou, China, 3Siemens Healthcare Ltd, Shanghai, China
Synopsis
This study aimed to compare the performance of different diffusion models of,including the mono-exponential, intravoxel incoherent motion (IVIM) model and the diffusion kurtosis imaging (DKI) model,for the correlation with molecular subtype and molecular prognostic factors. The results indicate that ADC, IVIM-D, DKI-D can be used to differentiate luninal B group from others molecular subtype. Quantitative MR diffusion parameters, such as ADC ,DKI-K, DKI-D , IVIM-FP and IVIM-D were significantly associated with HER2 overexpression, Ki-67 proliferation status and histological grade in patients with breast cancer.
Introduction
Heterogeneity is a known hallmark of breast cancer. In the age of personalized medicine, tumor heterogeneity is an important information in routine clinical practice, as different molecular subtypes show different characteristics of biological behavior, which leads to different the treatment methods and prognosis. As a functional imaging method, diffusion-weighted imaging can reflect the pathological information changes of the disease at the molecular level by measuring the fluidity of water molecules in the tissue. With the development of diffusion technology, the intravoxel incoherent motion (IVIM) model and the diffusion kurtosis imaging (DKI) model have been proposed and applied in many tissue types[1-3]. This study aimed to evaluate the diagnostic value of mono-exponential, IVIM and DKI models of DWI in correlation with molecular subtype and molecular prognostic factors.Methods
152 Patients who were clinically suspected to have a breast tumor and scheduled to receive fine-needle aspiration biopsy or surgical treatment between August 2019 and October 2020 were consecutively recruited in this study. All MR exams were performed on a 3T MRI scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) with a 18-channel breast coil. DW images (single-shot echo-planar imaging prototype sequence) with spectral attenuated inversion recovery for fat suppression were acquired with the following parameters: TR/TE = 5700/62ms, slice thickness = 4mm, slices = 35, bandwidth = 2024Hz/Px, FOV = 340x60mm2, b values of 0, 30, 50, 80, 120,160, 200, 500, 1000, 1500, and 2000 sec/mm2, the total acquisition time = 5min 8sec. ADC maps were automatically generated from conventional DWI with b values of 0 and 1000 sec/mm2 with the software integrated in the MR imager (Syngo; Siemens Healthcare, Erlangen Germany). Kurtosis coefficient (DKI-K) and diffusivity coefficient (DKI-D) were calculated from DKI with b values of 0, 500, 1000, 1500, and 2000 sec/mm2 ; molecular diffusion coefficient (IVIM-D), perfusion-related diffusion coefficient (IVIM-DP) and perfusion fraction (IVIM-FP) were calculated from IVIM with b values of 0, 30, 50, 80, 120, 160, 200, 500 and 1000 sec/mm2 by a prototype software, body diffusion toolbox (Siemens Healthcare, Erlangen, Germany). Histologic reports which evaluated the prognostic biomarker status of the breast cancer were reviewed. Tumor grades were then dichotomized into “low” (grades 1 and 2) and “high” (grade 3). Immunohistochemical staining results for estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2) were evaluated. The results were dichotomized into “positive” and “negative” . For assessing ER and PR, the Allred scoring system was used and a score of more than 2 was considered positive[4]. HER2 overexpression was considered positive when membranes were graded 3+ or 2+ on immunohistochemistry, with HER2 gene amplification in silver-stained in situ hybridization. The Ki67 index was determined to be positive if the expression was 20%. According to the ER, PR, HER2, and Ki67 results,molecular subtypes of breast cancers were classified into “luminal A” , “luminal B(HER2+)”, “luminal B(HER2-)” , “HER2-overexpression,” or “Basal-like” [5]. For data analysis, quantitative variables are shown as mean ± standard deviation. Two independent samples t-tests were used to compare normal distribution data, and the Mann–Whitney U test was used to compare nonnormal distribution parameters from DWI (ADC), DKI (MK, MD)and IVIM (IVIM-FP, IVIM-D, IVIM-DP), between the“positive” and “negative”prognostic biomarker status based on histopathologic results as the gold standard. Statistical significance was defined as p ≤ 0.05.Results
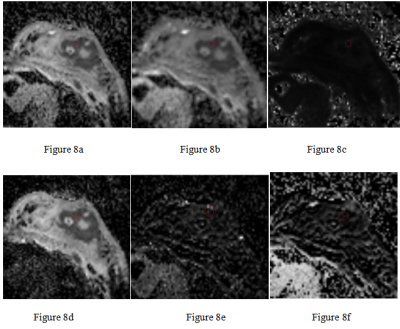
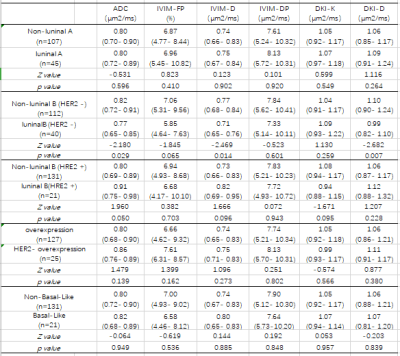
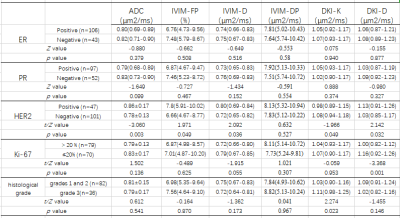
The results demonstrated that ADC, IVIM-D, DKI-D showed statistically differencesd between luninal B(HER2 -) and Non-luninal B(HER2 -)(P<0.05)(Table 1) using MW test. Similarly, ADC value showed statistically differentiation for the luninal B(HRE2 +) group and others by MW testing (p=0.05)(Table1). ADC, IVIM-FP, IVIM-D, DKI-K, DKI-D showed statistically differences between HER2-positive and HER2-negative status(P=0.003, 0.049, 0.036, 0.049, 0.032, respectively). The DKI-D value (1.00(0.82-1.12)) of Ki-67-positive status was significantly lower than that (1.16(0.92-1.26)) of Ki-67-Negative (P=.0001). In addition, DKI-K value also statistically differentiated between different histological grade. There were no significant differences among all diffusion parameters in estrogen or progesterone receptor “positive” and “negative” (P>0.05). (Table 2)(Figure1-7) The calculated quantitative maps of the representative patients were shown in Figure 8.Conclusions
The results of this study suggests that ADC, IVIM-D, DKI-D can be used to differentiate luninal B group from others molecular subtype. Quantitative MR parameters, such as ADC derived from standard DWI, DKI-K and DKI-D derived from DKI ,and IVIM-FP, IVIM-D derived from IVIM, were significantly associated with HER2 overexpression, Ki-67 proliferation status and histological grade in patients with breast cancer.Acknowledgements
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was not required because this was a retrospective study. No study subjects or cohorts have been previously reported.
References
1. Zebin Xiao, Yufeng Zhong, Zuohua Tang, et al. Standard diffusion-weighted, diffusion kurtosis and intravoxel incoherent motion MR imaging of sinonasal malignancies: correlations with Ki-67 proliferation status[J]. Eur Radiol, 2018 28(7):2923-2933.
2. Yingchan Shan, Xiaoshan Chen, Kai Liu, et al. Prostate cancer aggressive prediction: preponderant diagnostic performances of intravoxel incoherent motion (IVIM) imaging and diffusion kurtosis imaging (DKI) beyond ADC at 3.0 T scanner with gleason score at final pathology[J].Abdom Radiol (NY), 2019 , 44(10) : 3441- 3452.
3. Huan Zhang, Wenhua Li, Caixia Fu, ea al. Comparison of intravoxel incoherent motion imaging, diffusion kurtosis imaging, and conventional DWI in predicting the chemotherapeutic response of colorectal liver metastases[J]. Eur J Radiol, 2020, 130: 109149.
4. M Elizabeth H Hammond, Daniel F Hayes, Mitch Dowsett, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridgedversion)[J].Arch Pathol Lab Med, 2010, 134(7):e48-72.5.
5. A Goldhirsch, E P Winer, A S Coates, et al. Personalizing the treatment of women with early breast cancer: highlights of the st gallen international expert consensus on the primary therapy ofearly breast cancer[J]. 2013, 24(9):2206-2223.
Figures
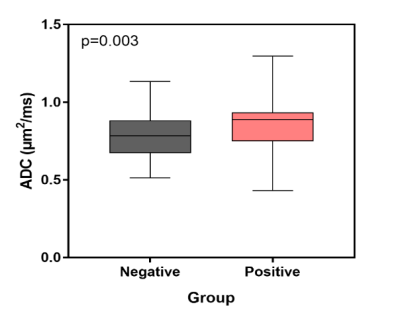
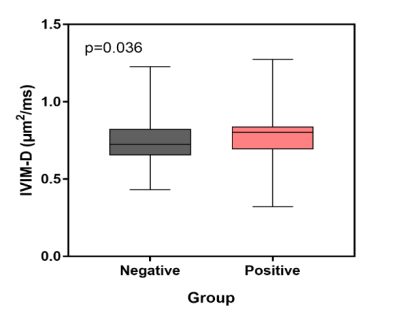

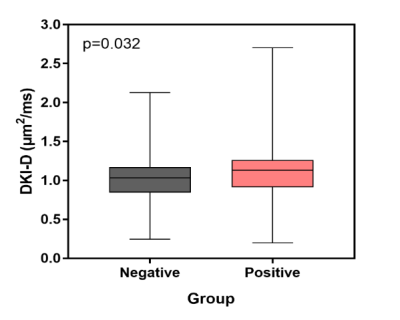
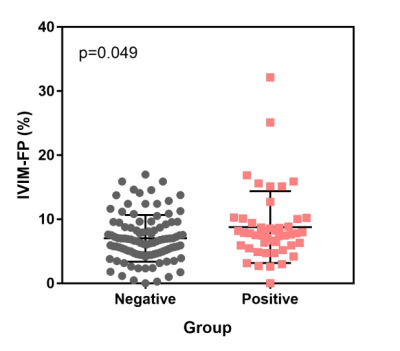
Figure5
Figure 1-5. Boxplots and Scatterplots show ADC, IVIM-D, DKI-K, DKI-D and IVIM-FP distribution of HER2-positive and HER2-negative status. Figure 1-4. The mean ADC, IVIM-D, DKI-K, DKI-D and IVIM-FP values of these two sets of statistical measurements are: positive: 0.86, 0.80, 0.93, 1.13μm2/ms, 7.8% and negative: 0.78, 0.72, 1.08, 1.03 μm2/ms, 6.66%. (Wilcoxon rank-sum test, p<0.05).
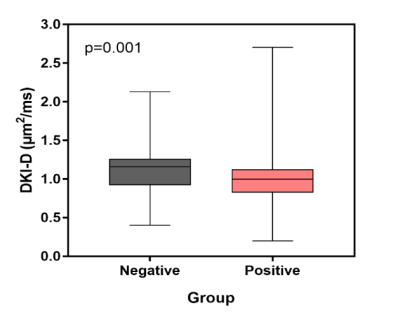
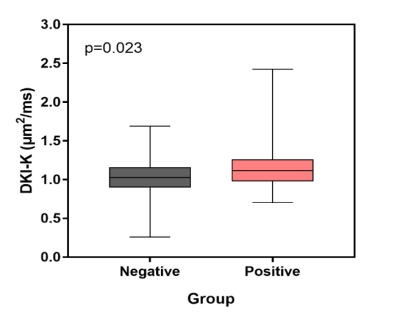
Figure 7. Boxplots show the mean DKI-K value of histological grade1, 2 and 3 are: grade1, 2 1.03 μm2/ms, grade31.11 μm2/ms.