1129
Feasibility of Using a Deep Learning Reconstruction to Increase Protocol Flexibility for Breast MRI1Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 2Radiology, University of Wisconsin-Madison, Madison, WI, United States, 3Global MR Applications and Workflow, GE Healthcare, Madison, WI, United States, 4Carbone Cancer Center, University of Wisconsin-Madison, Madison, WI, United States
Synopsis
A deep learning reconstruction was evaluated for use in T2w breast MRI. Breast radiologists scored deep learning (DL) images significantly higher than non-DL images in four categories: artifacts, perceived signal-to-noise ratio, sharpness, and overall quality. DL was then used to improve the quality of high-resolution T2w breast series acquired in clinically-acceptable scan times. High resolution protocols typically require compromise between scan time and image quality. However, implementation of a deep learning reconstruction allowed for shorter scan times while maintaining diagnostic image quality. A deep learning reconstruction could allow for a clinically-feasible, high-resolution T2w acquisition.
Introduction
Recent advances in deep learning (DL) reconstruction for MRI have produced a myriad of trained neural networks capable of increasing the quality of diagnostic images.1,2,3 However, networks can be limited by lack of diversity in the training data prohibiting widespread use. In our work, we use a prototype DL reconstruction that is anatomically non-specific and based upon a convolutional neural network trained to denoise, sharpen, and remove simple artifacts from images.4 This allows for greater flexibility in choosing an acquisition to be paired with the DL reconstruction.One approach is to incorporate DL reconstructions into existing clinical protocols. While this would improve image quality, patients may see limited benefit especially if the conventional, non-DL images are diagnostically sufficient. Alternatively, it may be possible to leverage DL to overcome classical MRI tradeoffs of resolution, signal-to-noise ratio (SNR), and scan time. Previous analysis in breast imaging explored decreasing acquisition time using a single-shot fast spin echo acquisition with DL.5
In this work, we examine radiologists' perception of conventionally-acquired T2-weighted (T2w) breast images produced using DL. We then demonstrate the feasibility of obtaining diagnostic quality images using a high-resolution protocol in conjunction with DL to achieve clinically-acceptable scan times.
Methods
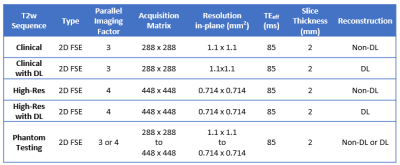
DL EvaluationPatients undergoing routine clinical breast MRI on a 3.0T scanner (Discovery 750w, GE Healthcare, Waukesha, WI) using a 16-channel breast coil (Sentinelle, Invivo International, Gainsville, FL) were evaluated. Clinical 2D T2w FSE images were obtained using the scan parameters found in Table 1. Images were reconstructed in two ways: using the conventional pathway included with the MR scanner (non-DL) and using a DL-based, vendor-provided prototype (DL).
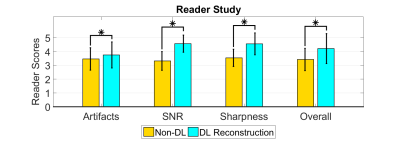
Four breast radiologists (two experienced faculty and two breast imaging fellows) scored the quality of all images. A 5-point scale was used to rate perceived SNR, perceived sharpness, presence of artifacts, and overall quality from 1 (poor, non-diagnostic quality) to 5 (highest quality). Readers also indicated a preferred series, either non-DL or DL. Differences in image quality scores were tested for significance using a Wilcoxon Rank-Sum test.
High-Resolution Clinical Add-on
Patients presenting for routine clinical breast MRI were consented to undergo an additional research MRI acquisition for this IRB-approved, HIPAA compliant study. Imaging was performed on a 3.0T MRI scanner (Signa Premier, GE Healthcare) using a 448 x 448 acquisition matrix and in-plane resolution of 0.714 x 0.714 mm2 matching the resolution of the T1w series of the breast MRI exam. Non-DL and DL reconstructions were performed. Two breast radiologists reviewed the DL series for diagnostic quality.
High-Resolution Phantom Study
A resolution phantom was scanned using a 21-channel head-and-neck coil (GE Healthcare) on a 3.0T MRI scanner (Signa Premier) to evaluate DL performance with increased acquisition matrices. First, the phantom was imaged using a protocol similar to the clinical T2w breast acquisition. Then, parallel imaging acceleration was increased from 3 to 4 and the acquisition matrix was systematically increased to achieve resolutions from 1.1 x 1.1 mm2 to 0.714 x 0.714 mm2. Data were reconstructed to obtain non-DL and DL images. SNR was measured using the same method as Lebel.4 Image sharpness was quantified as the maximum slope of line profiles taken across abrupt phantom edges. The ratio of maximum slope between non-DL and DL images was calculated.
Results
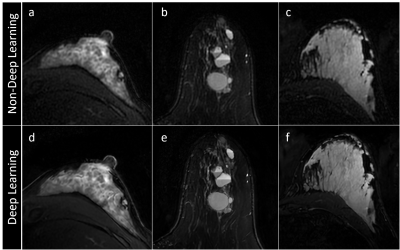
DL EvaluationConventional T2w series from twenty consecutive clinical breast exams were used for DL evaluation. Two cases had bilateral breast implants and two cases had a single implant. Three examples are shown in Figure 1. Radiologists found that DL significantly improved each image quality metric assessed (Figure 2): presence of artifacts (p=0.01), perceived sharpness (p<0.01), SNR (p<0.01), and overall image quality (p<0.01). Although, in some instances artifacts present in the non-DL series were accentuated in the DL series. In 15 of 20 cases (75%), all four radiologists preferred the DL over non-DL series.
High-Resolution Clinical Add-on
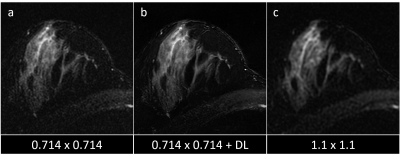
Two additional patients underwent an additional high-resolution T2w sequence. Radiologists stated that images were of sufficient diagnostic quality. The increase in acquired spatial resolution lengthened mean imaging time (199 to 245 seconds). An example case can be found in Figure 3.
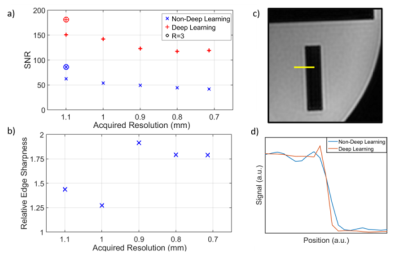
High-Resolution Phantom Study
Phantom results are shown in Figure 4. The DL reconstruction achieved at least 2.1 times the SNR of non-DL images. Additionally, DL images had a 1.3 to 1.9 times greater sharpness with a greater increase at higher resolutions.
Discussion
The DL reconstruction provided significant improvements in perceived SNR, image sharpness, and overall image quality for T2w images compared with non-DL images. Application of DL to a high-resolution imaging protocol provided diagnostic quality images requiring only a modest increase in scan time (<1 minute). Our findings demonstrate a departure from the traditional trade-off of scan time, resolution, and SNR. While the trade-off still exists, its impact is diminished.The DL reconstruction was found to sharpen and enhance both desired imaging features as well as motion-related artifacts. It is important to be aware of this during image interpretation.
Conclusions
The DL reconstruction provided a flexible tool for increasing SNR and sharpness with significant improvements in image quality observed in vivo. Application of the DL allowed for acquisition of high-resolution images with only a modest increase in scan time.Acknowledgements
This project was supported by the Departments of Radiology and Medical Physics, University of Wisconsin-Madison.References
1. Higaki, T., Nakamura, Y., Tatsugami, F., Nakaura, T., & Awai, K. (2019). Improvement of image quality at CT and MRI using deep learning. Japanese Journal of Radiology, 37(1), 73–80. https://doi.org/10.1007/s11604-018-0796-2
2. Chen, F., Taviani, V., Malkiel, I., Cheng, J. Y., Tamir, J. I., Shaikh, J., Chang, S. T., Hardy, C. J., Pauly, J. M., & Vasanawala, S. S. (2018). Variable-density single-shot fast spin-echo MRI with deep learning reconstruction by using variational networks. Radiology, 289(2), 366–373. https://doi.org/10.1148/radiol.2018180445
3. Xie, D., Li, Y., Yang, H., Bai, L., Wang, T., Zhou, F., Zhang, L., & Wang, Z. (2020). Denoising arterial spin labeling perfusion MRI with deep machine learning. Magnetic Resonance Imaging, 68(January), 95–105. https://doi.org/10.1016/j.mri.2020.01.005
4. Lebel, R.M. Performance characterization of a novel deep learning-based MR image reconstruction pipeline. August 2020. http://arxiv.org/abs/2008.06559
5. Allen T, Henze Bancroft LC, et al. Shortening Diagnostic T2w Breast Protocols to Capitalize on the Benefits of a Deep Learning Reconstruction [abstract]. 27th Annual Meeting of the International Society of Magnetic Resonance in Medicine; 2020 Aug 8-14.
Figures