1125
A BI-RADS like lexicon for Breast DWI: Proposal and early evaluation1Diagnostic Imaging and Nuclear Medicine, Kyoto University Graduate School of Medicine, Kyoto, Japan, 2Clinical Innovative Medicine, Institute for Advancement of Clinical and Translational Science, Kyoto University Hospital, Kyoto, Japan, 3Radiology, Kitano Hospital, The Tazuke Kofukai Medical Research Institute, Osaka, Japan, 4Breast Surgery, Kitano Hospital, The Tazuke Kofukai Medical Research Institute, Osaka, Japan
Synopsis
Our proposed DWI reading method based on the BI-RADS lexicons from multiple b-value images had comparable specificity and NPV to the standard BI-RADS. The DWI reading method might increase diagnostic confidence in differentiating malignant and benign breast tumors. Excellent to substantial agreement was observed for DWI reading. Substantial-perfect agreement was observed in lesion characteristics and fibrograndular tissues, according to an adjusted BI-RADS lexicon for lesion classification. These results suggest that DWI reading methods might be applicable in a clinical setting, however, the agreement is moderate for non-mass lesions, which is still challenging for clinical application.
Introduction
The utility of DWI has been widely investigated for the diagnosis and monitoring of breast lesions, however, it is not included in the BI-RADS-MRI assessment1-3, and international efforts are underway to standardize breast DWI4. Evaluation of breast tumor morphology by DWI has been also investigated5, 6,with overall moderate agreement based on BI-RADS lexicons between DWI and DCE-MRI-reading . DW images using multiple b values have been mainly investigated as a quantitative rather than qualitative approach, such as IVIM and non-gaussian DWI3. However, there has been no studies investigating the qualitative utility of DW images using multiple b values so far as we know. Interpretation of DW images using multiple b values could also be worthy of investigation, which can omit the processing step and might add the diagnostic merit from DW images both at low and high b values in breast cancer characterization. Hence, we propose a DWI-reading method based on the BI-RADS lexicons from multiple b-value images (b=0,200,800,1000,1500 sec/mm2). Diagnostic performance for differentiating malignancy and non-malignancy was evaluated in comparison with standard BI-RADS (using DCE).Materials & Methods
-Study design and MRI acquisition-This prospective study was approved by our institutional review board and included 104 women suspected of breast cancer. 197 breasts were read by two independent radiologists. 95 breast lesions were suspected on breast MRI in the clinical setting, and 62 breast tumors biopsied (39 malignant and 23 benign). Flow chart and lesions characteristics are shown in Figure 1. Breast MRI was performed using a 3-T system (Achieve 3T; Philips) equipped with a dedicated 7-channel breast array coil. DWI was acquired using five b-values of 0, 200, 800, 1000, and 1500 s/mm2; repetition time/echo time, 12 500/79 ms; flip angle, 90°; field of view, 350 × 350 mm; matrix, 112×145; slice thickness, 4.0 mm; and acquisition time, 6 min 15 s.
-DWI-based and BI-RADS reading-
An adjusted BI-RADS lexicon for lesion classification was established to accommodate to DWI-based reading, as investigated previously7 (Table 1). Two radiologists A and B independently assessed lesion characteristics and normal breast tissue solely on the DW images using all five b-values of 0, 200, 800, 1000, and 1500 s/mm2 according to an adjusted BI-RADS lexicon for lesion classification. ADC maps were available. Qualitative evaluation of signal intensities on DW images for each b value was also considered for lesion classification (example shown in Figure 2; remaining signal at high b values suggestive for malignancy, diminishing signal at high b values suggestive of non-malignancy).
The readers were blinded to all clinical information, findings on other imaging modalities, pathological diagnosis, and other reader’s interpretations. This was followed by a standard reading including DCE. Fibroglandular tissue (FGT) assessment on DWI was made using the b=0 s/mm2 DW image. BI-RADS category 1-3 were classified as non-malignant, and BI-RADS category 4 and 5 were classified as malignant. Diagnostic performance was evaluated using ROC analysis. Kappa statistics were calculated to measure interobserver agreement in breast DWI between two radiologists.
Results
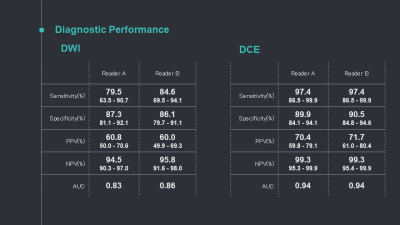
Representative cases are shown in Figure 2. Signal at high b values tended to remain at high b values in malignant tumors, while some benign tumors showed marked signal intensity at low b-value, decreasing at high b-value. Diagnostic performance for DWI and DCE-MRI is shown in Table 2. Overall, sensitivity and PPV tended to be inferior with DWI (80-61% and 85-60% for each radiologist, respectively) than with DCE-MRI (97-70% and 97-72%), while specificity and NPV were comparable (87-95% and 86-96% for DWI, 90-99% and 91-99% for DCE-MRI). Substantial-perfect agreement for BI-RADS categories and mass characteristics (0.83-0.93) and the agreement was moderate for non-mass distribution (0.44).Discussion
Sensitivity and PPV tended to be inferior with DWI than with DCE-MRI, while specificity and NPV were comparable in our study. Higher specificity and lower sensitivity in DWI was reported in the literature8. With comparable NPV, DWI reading with multiple b-values has the potential to increase diagnostic confidence in differentiating malignant and benign breast tumors. The signal in malignant tumors tends to be observable on both b=1000 and 1500 s/mm², while the signals almost disappear at 1500 s/mm² in many benign tumors, which may also provide confidence in tumor characterization. Very high b value of 1200-1500 is recommended to maximize lesion contrast, which was in agreement with previous investigations, including synthetic high b-values9,10. Substantial-perfect agreement was observed in lesion characteristics and fibrograndular tissues, according to an adjusted BI-RADS lexicon for lesion classification. The previous literature showed substantial-perfect agreement, comparable or superior to the previous study.6 These results suggest that DWI reading methods might be applicable in a clinical setting, however, the agreement is moredate for non-mass lesions, which is still challenging for clinical application.Conclusion
DWI reading methods showed comparable specificity and NPV to standard BI-RADS, and they might increase diagnostic confidence in differentiating malignant and benign breast tumors.Acknowledgements
This work was supported by AMED grant number under Grant Number JP18ck0106454. We would like to thank Maya Honda, Akane Ohashi, Rie Ota and Denis Le Bihan for their valuable advice.References
1. Shi RY, Yao QY, Wu LM, Xu JR. Breast Lesions: Diagnosis Using Diffusion Weighted Imaging at 1.5T and 3.0T-Systematic Review and Meta-analysis. Clin Breast Cancer. 2018; 18:e305-e320.
2. Zhang L, Tang M, Min Z, Lu J, Lei X, Zhang X. Accuracy of combined dynamic contrast-enhanced magnetic resonance imaging and diffusion-weighted imaging for breast cancer detection: a meta-analysis. Acta radiologica. 2016; 57:651-660.
3. Iima M, Honda M, Sigmund EE, Ohno Kishimoto A, Kataoka M, Togashi K. Diffusion MRI of the breast: Current status and future directions. Journal of Magnetic Resonance Imaging. 2020; 52:70-90.
4. Baltzer P, Mann RM, Iima M, et al. Diffusion-weighted imaging of the breast-a consensus and mission statement from the EUSOBI International Breast Diffusion-Weighted Imaging working group. Eur Radiol. 2020; 30:1436-1450.
5. Radovic N, Ivanac G, Divjak E, Biondic I, Bulum A, Brkljacic B. Evaluation of Breast Cancer Morphology Using Diffusion-Weighted and Dynamic Contrast-Enhanced MRI: Intermethod and Interobserver Agreement. J Magn Reson Imaging. 2018.
6. Kul S, Metin Y, Kul M, Metin N, Eyuboglu I, Ozdemir O. Assessment of breast mass morphology with diffusion-weighted MRI: Beyond apparent diffusion coefficient. J Magn Reson Imaging. 2018; 48:1668-1677.
7. Kishimoto AO, Kataoka M, Iima M, et al. The comparison of high-resolution diffusion weighted imaging (DWI) with high-resolution contrast-enhanced MRI in the evaluation of breast cancers. Magnetic Resonance Imaging. 2020; 71:161-169.
8. Daimiel Naranjo I, Lo Gullo R, Saccarelli C, et al. Diagnostic value of diffusion-weighted imaging with synthetic b-values in breast tumors: comparison with dynamic contrast-enhanced and multiparametric MRI. European Radiology. 2020.
9. Park JH, Yun B, Jang M, et al. Comparison of the Diagnostic Performance of Synthetic Versus Acquired High b-Value (1500 s/mm(2) ) Diffusion-Weighted MRI in Women With Breast Cancers. J Magn Reson Imaging. 2019; 49:857-863.
10. Jendoubi S, Wagner M, Montagne S, et al. MRI for prostate cancer: can computed high b-value DWI replace native acquisitions? European Radiology. 2019; 29:5197-5204.
Figures
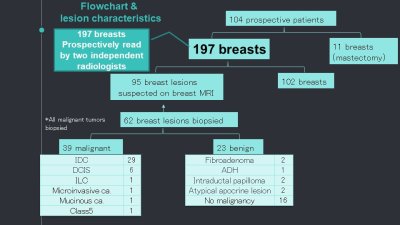
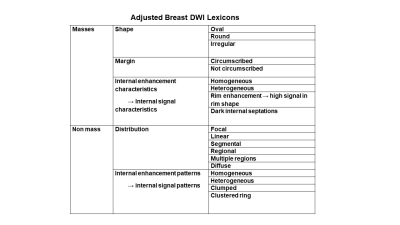
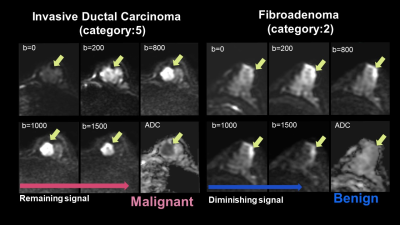
Figure 2:
the representative case of the typical malignant tumor (left). The tumor shows moderate signal intensity at low b-value, an increased signal at high b-value, and decreased ADC, suggesting malignancy. Invasive ductal carcinoma.
the representative case of the typical benign tumor (right). The tumor shows marked signal intensity at low b-value, decreased signal at high b-value, and slightly low ADC, suggesting a benign breast tumor. Fibroadenoma.