1124
A Comparison of different models of diffusion-weighted MRI in distinguishing benign and malignant breast lesions1Radiology, Provincial Clinical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou, China, 2Siemens Healthcare Ltd, Shanghai, China
Synopsis
This study aims to analyze the value of ADC, IVIM and DKI in differentiating benign and malignant breast nodules. The combination of all the quantitative diffusion parameters is also evaluated. The value of ADC, IVIM-D, KDI-K and DKI-D can be used as a diagnostic tool for evaluating benign and malignant breast lesions. Compared with IVIM-D, DKI-K and DKI-D, ADC value is the best single discriminative parameters to differentiate breast lesions. Further, the combination of ADC and DKI-K value shows the best diagnostic efficacy.
Introduction
In recent years, the value of conventional quantitative diffusion, i.e. apparent diffusion coefficient (ADC), in the differentiation of benign and malignant breast nodules has been proven. Recently, advanced multi b value diffusion post processing model, such as intravoxel incoherent motion (IVIM) and diffusional kurtosis imaging (DKI), are reported to be useful in distinguishing benign and malignant tumor in liver, prostate and sinus tumor (1-3). However, there are few literatures compare ADC, IVIM and DKI for breast tumor in one study. Therefore, this study aim to analyze the value of ADC, IVIM and DKI in differentiating benign and malignant breast nodules. The combination of all the quantitative diffusion parameters is also evaluated.Methods
From June 2019 to October 2020, 215 lesions from 202 female patients(mean age, 49.7 years; range, 27–80 years) were enrolled in this study, including 152 cases of malignant lesions and 63 cases of benign ones, which were confirmed pathologically and clinically. All MR exams were performed on a 3T MRI scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) with an 18-channel breast coil. The parameters of the DWI sequences was: TR/TE =5700/62/ms, slice thickness = 4 mm, number of slices = 35, bandwidth =2024 Hz/Px, FOV = 340 × 60 mm2, b = 0, 30, 50, 80, 120, 160, 200, 500,1000, 1500 and 2000 sec/mm2, acquisition time = 5 min 08s. The ADC value were calculated using the b values of 0 and 1000 sec/mm2, the IVIM parameters were obtained using the b value of 0, 30, 50, 80, 120, 160, 200, 500, and 1000 sec/mm2 and the DKI parameters were acquired using the b values of 0, 500, 1000, 1500 and 2000 sec/mm2. The post-processing was performed by a prototype software, body diffusion toolbox, (Siemens Healthcare, Erlangen, Germany) to obtain the following quantitative parameters: 1) apparent diffusion coefficient (ADC), 2) perfusion fraction (IVIM-FP), 3) molecular diffusion coefficient (IVIM-D), 4) pseudo-diffusion coefficient, IVIM-DP) , 5) mean kurtosis (DKI-K), 6) mean diffusivity (DKI-D). All quantitative parameter between benign and malignant lesions were measured three times based on the regions of interest (ROI) depicted on the lesions. Quantitative variables are shown as mean ± standard deviation. Two independent samples t-tests were used to compare normal distribution data, and the Mann–Whitney U test was used to compare nonmoral distribution parameters from DWI (ADC), DKI (DKI-K, DKI-D) and IVIM (IVIM-FP, IVIM-D, IVIM-DP). Receiver operating characteristic (ROC) curve analysis was used to determine the diagnostic value of quantitative parameters for differentiating benign and malignant lesions. Optimal cutoff points were estimated for each parameter, according to the point on the ROC curve with the maximum Youden index. The sensitivity, specificity, accuracy values of the qualitative and quantitative parameters were calculated, with 95% confidence intervals, using a standard formula.Results
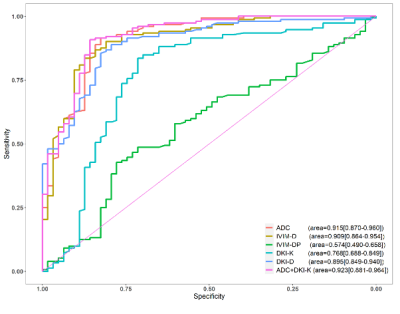
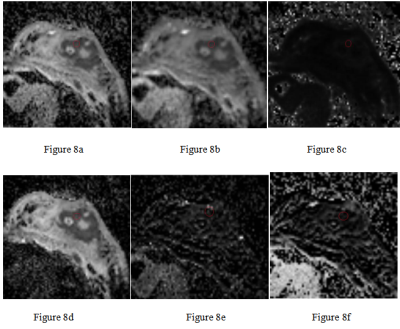
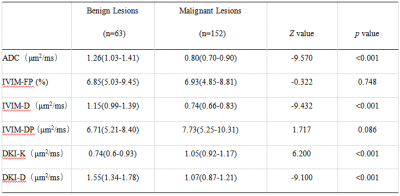
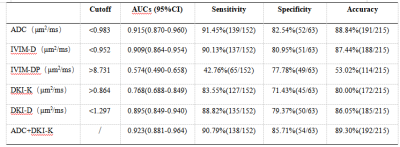
According to the statistic results, ADC, IVIM-D, DKI-K and DKI-D value show significant differences between the benign and malignant lesions(p<0.001) (Table 1) (Figure1-6). The best quantitative parameter is ADC, which enjoyes the highest sensitivity(91.45%), specificity(82.54%) and accuracy(88.84%) (table 2). The area under the ROC curve (AUC) of ADC value is 0.915 with the optimal cut-off point is 0.983 μm2/ms. The combined application of ADC and DKI-K shows the best diagnostic effectiveness. It has sensitivity (90.79%), specificity (85.71%) , accuracy(89.30%) and AUC (0.923) (Figure 7). The calculated quantitative maps of the representative patient were shown in Figure 8.Conclusions
The value of ADC, IVIM-D, KDI-K and DKI-D can be used as a diagnostic tool for evaluating benign and malignant breast lesions. Compared with IVIM-D, DKI-K and DKI-D, ADC value is the best single discriminative parameters to differentiate breast lesions. Further, the combination of ADC and DKI-K value shows the best diagnostic efficacy.Acknowledgements
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was not required because this was a retrospective study. No study subjects or cohorts have been previously reported.References
1. Zebin Xiao, Yufeng Zhong, Zuohua Tang, et al. Standard diffusion-weighted, diffusion kurtosis and intravoxel incoherent motion MR imaging of sinonasal malignancies: correlations with Ki-67 proliferation status[J]. Eur Radiol, 2018 28(7):2923-2933.
2. Yingchan Shan, Xiaoshan Chen, Kai Liu, et al. Prostate cancer aggressive prediction: preponderant diagnostic performances of intravoxel incoherent motion (IVIM) imaging and diffusion kurtosis imaging (DKI) beyond ADC at 3.0 T scanner with gleason score at final pathology[J].Abdom Radiol (NY), 2019 , 44(10) : 3441- 3452.
3. Huan Zhang, Wenhua Li, Caixia Fu, ea al. Comparison of intravoxel incoherent motion imaging, diffusion kurtosis imaging, and conventional DWI in predicting the chemotherapeutic response of colorectal liver metastases[J]. Eur J Radiol, 2020, 130: 109149.
Figures
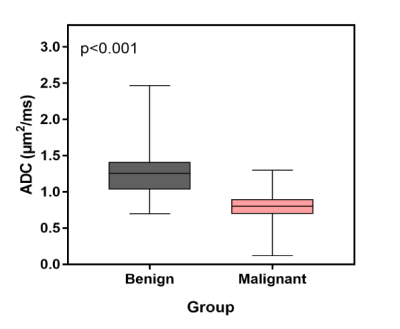
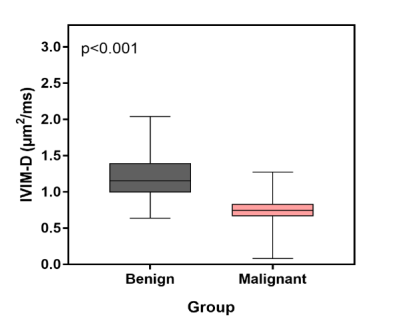
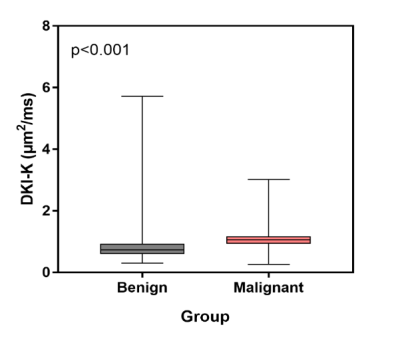
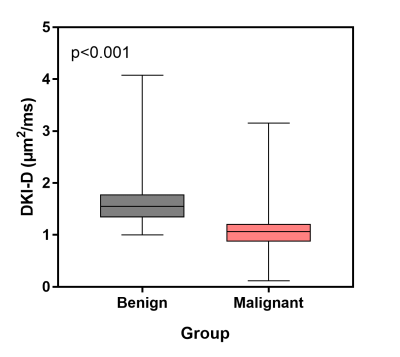
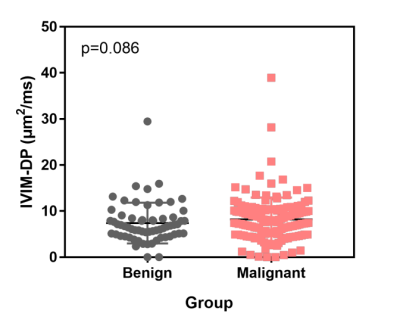
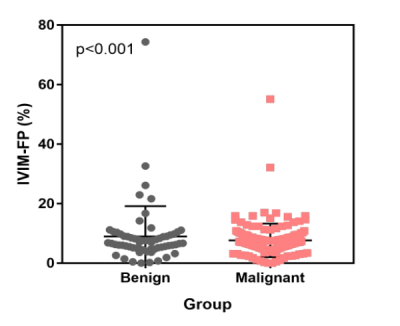
Figure6
Figure 1-6. Boxplots and Scatterplots show ADC, IVIM-D, DKI-K, DKI-D, IVIM-DP and IVIM-FP distribution of benign and malignant breast lesions. Figure 1-4. The mean ADC, IVIM-D, DKI-K, and DKI-D values of these two sets of statistical measurements are: benign: 1.26, 1.15, 0.74, 1.15 μm2/ms and malignant: 0.80, 0.74, 1.05, 1.07 μm2/ms. (Wilcoxon rank-sum test, p<0.001). Figure 5-6. The mean IVIM-DP and IVIM-FP values of these two sets of statistical measurements are: benign: 6.71 μm2/ms, 6.85% and malignant: 7.73 μm2/ms, 6.93% (Wilcoxon rank-sum test, p>0.05).