1123
Influence of gadolinium-based contrast agent on DWI and ADC values in breast lesions1Radiology, the Netherlands Cancer Institute – Antoni van Leeuwenhoek, Amsterdam, Netherlands, 2Medical Physics, the Netherlands Cancer Institute – Antoni van Leeuwenhoek, Amsterdam, Netherlands
Synopsis
It is advocated to perform breast DWI-acquisitions before contrast administration [1]. However, performing DWI after contrast MRI might be more practical in a clinical context. Several studies [2] evaluated whether performing breast MRI before or after contrast administration impacts the DWI classifying properties. However, previous research was often based on an interpatient analysis. Therefore, we performed a retrospective intra-patient analysis on perfusion-free ADC-maps before and after contrast administration. A decrease in ADC was observed in post-contrast ADC-values. This was independent of the B0-field strength, and similar for benign and malignant lesions.
Introduction
T1-weighted Dynamic Contrast-Enhanced Magnetic Resonance Imaging (DCE-MRI) is widely used for breast imaging. Moreover, other MRI-techniques as Diffusion-Weighted Imaging (DWI) [3] are continuously being optimized, to improve the clinical value of multiparametric breast MRI. DWI has obtained an important role in breast MRI to improve the classification of benign and malignant breast lesions. For quantitative evaluation of DWI, it is suggested to perform DWI examinations always prior to contrast administration. This results in an increase in scan time, indirectly depending on the magnitude, number of b-values, and Number of Signal Averages (NSA) chosen. In general, it implies that DWI will always substantially increase the duration of the scan protocol. Scan time is sparse and should be minimized for optimal efficiency and patient comfort. Alternatively, DWI might be acquired after contrast administration, which enables to obtain DWI only in patients with enhancing abnormalities. A further advantage is that DWI can be obtained during the wash-out period and thus hardly affect the total duration of the multiparametric protocol. Although this strategy seems beneficial, detailed analyses, regarding answering various clinical questions, remains limited. A systematic review of Dorrius et al. suggest a non-significant decrease in ADC after contrast administration based upon mostly inter-patient comparisson. [2] However, it is well known that ADC is vulnerable to a variety of aspects, such as sequence parameters, hardware, scan-moments, etc. Therefore, comparing separate patient groups with either a pre- or post-contrast DWI-scans might be challenging. To overcome this limitation, an intra-patient analysis was performed to investigate if a change in the lesion ADC was observed after injecting gadolinium based contrast agent, within the same scan session. We also assessed the impact on lesion classification.Materials and Methods
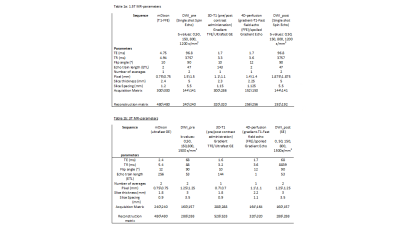
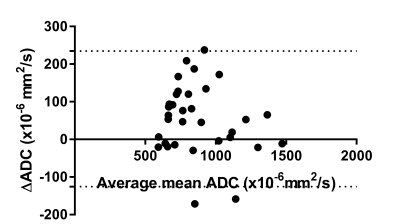
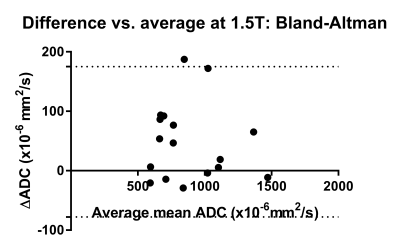
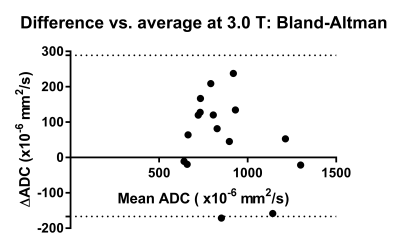
We included 31 patients in this analysis. Expansion of this cohort is pending. In all cases, DWI’s were acquired with parallel imaging (SENSE) and SPectral Attenuated Inversion Recovery (SPAIR) fat suppression before and after contrast administration during wash-out (roughly 2 min after contrast administration), within the same session on either a 1.5 T or 3.0 T MRI-scanner (Philips Healthcare, Best, The Netherlands), see table 1. Variations in image quality were present due to differences in gradient systems and coils (7-channel or 16-channel), however for each patient the sequence was always identical. In between both DWI’s, DCE-MRI was performed using a gadolinium-based contrast agent (CA) Dotarem ® . Lesions were detected using subtraction images obtained from the first 3D-T1 scan after contrast injection in combination with the 3D-T1 scan before contrast. Apparent Diffusion Coefficient (ADC)-maps were calculated on the scanner for both DWI acquisitions, using the b=150 s/mm2 and b=800 s/mm2 acquisitions to minimize the inclusion of perfusion effects within the mono-exponential (Gaussian) DWI-model. For post-processing, single slice Regions of interest (ROI) were drawn in the most apparent lesion (often index lesion) on the pre and post contrast high b-value image (b=1200 s/mm2 or 1500 s/mm2) separately, using the subtracted wash-in images as reference for lesion localization. Visual appearance of necrosis/fibrosis/markers resulted in the regional exclusions within the delineations. Furthermore, all voxels with diffusion values <0.5*10-3 mm2/s, considered as low outliers, were excluded from the ROI. For a first subset of cases pathological state was determined. Minimum, mean and maximum ADC values were extracted from the ROIs ADC-maps. For Statistical analysis, Bland-Altman plots were created with GraphPad Prism 7 for the difference in mean ADC for both benign and malignant lesions also taking the B0-field strength into account. Wilcoxon tests were used to compare groups, where significance was observed as p<0.05.Results
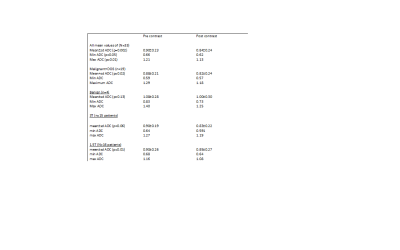
Thirty-three apparent lesions were analyzed. For 23 lesions pathological data was available, with 19 malignant and 4 benign lesions. On 1.5T scanner 15 patients were scanned and 16 patients on the 3.0 T-scanner. Delineated volumes on the pre-contrast ADC-maps after correcting low outliers, ranged from 25-3378 mm3. The post-contrast ADC volume range was 11-4273 mm3. Measured ADC values are reported in table 2 for the total group, based upon final diagnosis (malignant/benign), and split for the different field strengths. Corresponding Bland-Altman plots are shown in figure 1-3. For all lesions, a significant difference in mean ADC between pre and post contrast was observed (see table 2).Discussion
This preliminary analysis aims to answer the question whether ADC values change after contrast administration and if this impacts the clinical value of DWI. A decrease in ADC after contrast administration was observed. For all lesions, however this seems not to impact the differentiation between benign and malignant lesions. Whether this would influence the value of DWI in other settings, for example in the prediction of therapy response and prognostication remains to be answered. However, as the effect seems to be uniform over lesions of various histology this is not likely.Conclusion
Currently, preliminary data shows a decrease in ADC after contrast administration. However, the exact effect on specific lesions, and the effect on other clinical tasks such as therapy selection and patient stratification is currently still unclear.Acknowledgements
No acknowledgement found.References
[1] Baltzer P, Mann RM, Iima M, Sigmund EE, Clauser P, Gilbert FJ, Martincich L, Partridge SC, Patterson A, Pinker K, Thibault F, Camps-Herrero J, Le Bihan D; EUSOBI international Breast Diffusion-Weighted Imaging working group. Diffusion-weighted imaging of the breast-a consensus and mission statement from the EUSOBI International Breast Diffusion-Weighted Imaging working group. Eur Radiol. 2020 Mar;30(3):1436-1450. doi: 10.1007/s00330-019-06510-3.
[2] Dorrius MD, Dijkstra H, Oudkerk M, Sijens PE. Effect of b value and pre-admission of contrast on diagnostic accuracy of 1.5-T breast DWI: a systematic review and meta-analysis. Eur Radiol. 2014 Nov;24(11):2835-47. doi: 10.1007/s00330-014-3338-z.
[3] Iima M, Honda M, Sigmund EE, Ohno Kishimoto A, Kataoka M, Togashi K. Diffusion MRI of the breast: Current status and future directions. J Magn Reson Imaging. 2020 Jul;52(1):70-90. doi: 10.1002/jmri.26908.