1076
Application of Multiband SENSE SAGE EPI towards DSC MRI of Brain Tumors
Sudarshan Ragunathan1, Laura C Bell1, Ashley M Stokes1, Ekokobe Fonkem1, John P Karis1, and C Chad Quarles1
1Barrow Neurological Institute, Phoenix, AZ, United States
1Barrow Neurological Institute, Phoenix, AZ, United States
Synopsis
Multi-echo acquisition strategies have the advantage of simultaneous quantification of T1/T2* values in DCR MRI, and when combined with multiband strategies, could provide comparable spatiotemporal coverage as a single shot EPI dynamic scan. While there has been some work on SMS – SAGE acquisitions, this is potentially the first work that utilizes a SENSE reconstruction framework. We demonstrated that the CNR of MBSAGE with SENSE is similar to SAGE acquisitions, and that the dynamic CNR with respect to NAWM is on the order of or slightly higher than reported by some of the SMS-SAGE implementations in literature.
INTRODUCTION
Multiband (MB) or simultaneous multi-slice (SMS) implementations have been combined with multi-echo acquisitions recently for obtaining increased coverage and simultaneous T1/T2* quantification for dynamic susceptibility contrast (DSC) MRI in the brain. The SMS-Spin and Gradient Echo technique (SAGE) with joint virtual coil reconstruction1 was shown to provide similar spatiotemporal coverage as that of clinical EPI protocols and used GRAPPA based reconstruction, while a model-based reconstruction approach of the SMS-SAGE data was performed in the imaging of gliomas2. Additionally, SAGE acquisitions accelerated with a SENSE reconstruction framework have been performed for imaging brain and muscle3 , and in preclinical imaging4. In this work we highlight the initial data quality results from combining Multiband SENSE and SAGE (MBSAGE) EPI in healthy volunteers and patients with brain tumors.METHODS
Imaging data was obtained from 12 healthy volunteers and 6 patients using a scan protocol approved by the Institutional Review Board. All individuals were scanned on Philips 3T Ingenia scanners. A Gd-based contrast agent (CA) with given using a full dose preload and bolus injection scheme. Variable flip angle based T1 maps were generated for q = [20, 18, 16, 14, 12, 10, 8, 6, 4, and 2] degrees. The MBSAGE EPI was implemented as a dynamic protocol [∆X,∆Y:2.5,2.5 mm; ∆Z: 5mm; TE1-TE5: 8.0/29.9/65.0/86.8/106.0 ms; TR:1500; p.f:0.74, MB:3; SENSE:2] and the data was acquired during preload of CA injection in patients. The volunteer data was acquired without the CA injection for SNR calculations. The patients also underwent a single echo dynamic EPI scan during the main CA injection [∆X,∆Y:2.5,2.5 mm; ∆Z: 5mm; TE:30ms; TR:1400 ms; SENSE : 2.3; p.f.: 0.732]. The image acquisitions were performed using a 15 channel head coil.Opposed phase EPI data were acquired for distortion correction. The MBSAGE data in volunteers and patients were registered to high resolution T1 anatomical acquisition. MBSAGE based ∆R1, ∆R2 and ∆R2* parameters were calculated as described in literature5. Contrast to Noise Ratio (CNR) was used as the data quality metric. In volunteers, CNR was obtained for Gray/White matter contrast (G-W CNR) and defined as $$$(G_M-W_M) CNR = \frac{|S.I.(W_M) – S.I.(G_M)|}{\sigma_{background air}}$$$. The average standard deviations (stdev) through time were obtained for Gray/White matter regions. In patient data, dynamic CNR (dCNR) was obtained as the ratio of max(∆R2*(t) or ∆R2(t)) and stdev of baseline signal before bolus passage. All data post-processing and analysis was performed in MATLAB (MathWorks Inc.).
RESULTS and DISCUSSION
Figure 1 shows the reconstructed MBSAGE echoes and their corresponding signal time curves in a representative gray matter voxel. Reconstruction errors arising due to residual aliasing in localized regions could be attributed to high multiband factor and low number of channels in the receive array. A 15 channel coil was used as standard in the clinical site and hence for our data acquisition. The distribution of Gray – White matter contrast shown in Fig. 2 was compared between sage acquisitions with and without multiband SENSE enabled. The CNR in the MBSAGE echoes was observed to be slightly lower than SAGE. Although, multiband reconstruction does not increase the g-factor noise, a combined multiband SENSE reconstruction can be influenced by coil sensitivity maps. Table 1 highlights the mean ± std of the CNR across the volunteers scanned. The variation in values could be explained from the low number of volunteers scanned. Dynamic CNR values in tumor patients are shown in Fig. 3. Figure 3A provides a boxplot of the dCNR obtained from gradient and spin echo relaxation time curves in the NAWM ROI in a tumor patient. A comparison of dCNR is shown for the 3 ROIs in Fig. 3B. The elevated levels of GM dCNR and WM dCNR could be influenced by partial volume effects and increased blood volume respectively. However, it is promising that the dCNR reported here are higher than those previously reported in literature (~16 – 20, for gradient echo and ~5 for spin echo)2. Future work would include comparison of CNR values with 32channel coil to study change in performance from the increase coil elements (which is expected with a SENSE reconstruction framework). Additionally, with this being an ongoing study, the next steps would be validating these quality metrics with the clinical standard of acquisition.Some of the limitations of this work include the low patient population, but as this is an ongoing study, more data will be acquired in the future. While this work presents healthy volunteer data, repeatability tests have to be carried out as part of the future work. Identifying areas of optimizing the multiband data acquisition would also help with improving some of the data quality metrics even further.
CONCLUSION
We have presented a SENSE based Multiband SAGE acquisition and reconstruction framework with comparable Gray-White matter contrast as SAGE acquisitions, promising dynamic CNR values and providing the same spatiotemporal coverage of a clinical EPI perfusion scan.Acknowledgements
This work was funded by the NIH/NCI 2R01 CA158079-01 grant award, and in part by Philips Healthcare.References
- Manhard MK, Bilgic B, Liao C, et al. Accelerated whole‐brain perfusion imaging using a simultaneous multislice spin‐echo and gradient‐echo sequence with joint virtual coil reconstruction. Magnetic Resonance in Medicine. 2019;82(3):mrm.27784. doi:10.1002/mrm.277842.
- Han M, Yang B, Fernandez B, et al. Simultaneous multi-slice spin- and gradient-echo dynamic susceptibility-contrast perfusion-weighted MRI of gliomas. NMR in Biomedicine. 2020;34(1). doi:10.1002/nbm.43993.
- Skinner JT, Robison RK, Elder CP, Newton AT, Damon BM, Quarles CC. Evaluation of a multiple spin- and gradient-echo (SAGE) EPI acquisition with SENSE acceleration: Applications for perfusion imaging in and outside the brain. Magnetic Resonance Imaging. 2014;32(10):1171-1180. doi:10.1016/j.mri.2014.08.0324.
- Stokes AM, Skinner JT, Quarles CC. Assessment of a combined spin- and gradient-echo (SAGE) DSC-MRI method for preclinical neuroimaging. Magnetic Resonance Imaging. 2014;32(10):1181-1190. doi:10.1016/j.mri.2014.08.0275.
- Schmiedeskamp H, Straka M, Newbould RD, et al. Combined spin- and gradient-echo perfusion-weighted imaging. Magnetic Resonance in Medicine. 2012;68(1):30-40. doi:10.1002/mrm.23195
Figures
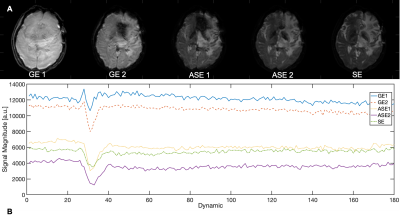
Figure 1: Each reconstructed echo from MBSAGE acquisition for an example brain tumor surveillance dataset is shown in (A). The corresponding signal intensity curves from a single gray matter voxel is shown in (B).
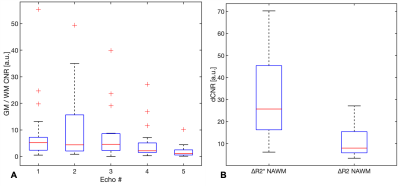
Figure 2: The gray-white matter contrast across healthy volunteers for each MBSAGE echo is shown in comparison to the SAGE CNR. Echo 2 showed the greatest contrast for SAGE and MBSAGE data with the median values being 376.9 and 287.9 respectively
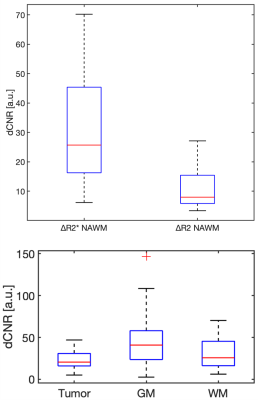
Figure 3: The dynamic CNR for change in transverse relaxation rates in an NAWM ROI are shown in (A) for the Gradient echo and Spin echo components of the MBSAGE data. Dynamic CNR in a tumor patient is shown for the 3 ROIs: tumor, gray matter and white matter, in (B).
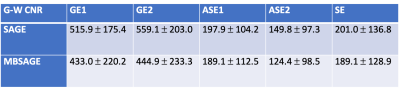
Table 1: Gray – White matter CNR values for each MBSAGE and SAGE echo across volunteers