0977
Left ventricular ejection fraction and global circumferential strain demonstrate non-linear relationship1University of Michigan, Ann Arbor, MI, United States, 2Medical College of Wisconsin, Milwaukee, WI, United States
Synopsis
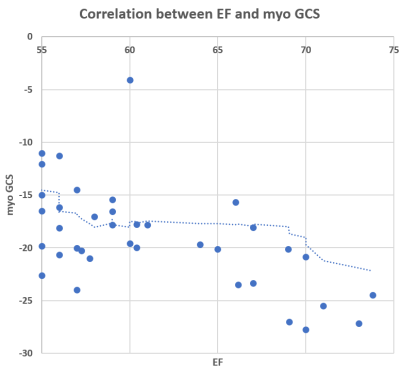
Left ventricular (LV) dysfunction as identified by depressed systolic function is an independent predictors of mortality and hospitalization with ischemic cardiomyopathy. LV systolic function as defined by the ejection fraction (EF) is quantified using cardiac imaging. We hypothesize that subset of patients with ischemic cardiomyopathy and normal LV EF of 55% demonstrate impairment in cardiac contractility by strain imaging. The results showed that the nonlinear relationship between LVEF and myocardium global circumferential-strain is indicative that EF is not sensitive to regional cardiac dysfunction or LV remodeling. Cardiac strain should become the cornerstone of the evaluation of patients with ischemic cardiomyopathy.
Introduction
Left ventricular (LV) dysfunction as identified by depressed systolic function is an independent predictors of mortality and hospitalization with ischemic cardiomyopathy. LV systolic function as defined by the ejection fraction (EF) is quantified using cardiac imaging. Cardiac magnetic resonance (CMR) is considered gold standard for quantifying LV systolic function which tailors the management of patients with ischemic cardiomyopathy. However, EF quantifies global LV function and does not take into account the regional wall motion abnormality that may potentially lead to LV remodeling and major adverse cardiac events. On the other hand, circumferential strain of the LV is more sensitive measure of contractile dysfunction than left ventricular ejection fraction and major contributor to LV stroke volume (Circulation, 112 (2005), pp. 984-991, Circulation, 118 (2008). Therefore, we hypothesize that subset of patients with ischemic cardiomyopathy and normal LV EF of 55% demonstrate impairment in cardiac contractility by strain imaging.Methods
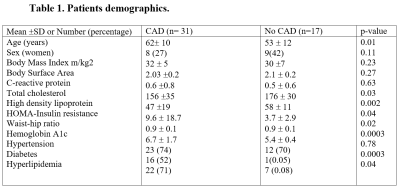
We prospectively recruited forty-nine patients from cardiac surgery clinics prior to their open heart surgery for coronary artery bypass grafting and valve repair. Mean body mass index (BMI) was 31 ± 6 kg/m2. All patients were stratified by the presence of CAD on coronary catheterization. All patients underwent fasting blood testing and cardiac MR imaging experiments performed on a 3T MR system (Philips Ingenia, Best, The Netherlands) in a 32-channel body coil. The protocol consisted of cine short-axis and long-axis images (steady-state with free precession (SSFP) sequence, repetition time (TR) = 4.2 ms, echo time (TE) = 1.8 ms, resolution = 1.4×1.4 mm2, slice thickness = 8 mm). A comprehensive cardiac MR protocol includes analyses of ventricular volume, function, and mass, including biventricular and left atrial strain and strain rate to assess contractility using feature tracking quantified with MEDIS software (Suite MR 7.6 Enterprise Solution, Leiden, Netherlands).Results
MR and CT imaging and fasting blood laboratory testing were performed on 49 patients (35% women) mean age 59±11 years, mean ejection fraction 58±9%, and mean heart rate of 73±14 beats per minute at the time of imaging. 29 (60%) patients had hyperlipidemia, 16 (33%) had diabetes. More than two thirds of the patients (73%) had hypertension and half (54%) had diastolic disfunction. CAD was present in 29 (60%) patients. Patients’ demographics stratified by CAD are included in Table 1. While systolic function was not associated with the presence of coronary artery disease, the normal EF (>55%) demonstrated non-linear relationship with global radial strain (GRS) and myocardial global circumferential strain (GCS) in our cohort. For example, in Figure 1 we demonstrate lot of patients classified normal by EF (>55%), while strain is > -17% (range from -10% to -17%)), i.e. abnormal myocardial contractility.Conclusions
The nonlinear relationship between LV EF and myocardium GCS is indicative that EF is not sensitive to regional cardiac dysfunction or LV remodeling. Cardiac strain should become the cornerstone of the evaluation of patients with ischemic cardiomyopathy.Acknowledgements
No acknowledgement found.References
1. Nagel et al. Herz. 45:446-452
2. Sokolska et al. Kardiol Pol. 77(12):1123-1133.
3. Ibrahim. Heart Mechanics. MRI. CRC Press, Boca Raton, FL 2017.