0975
Single-shot Compressed Sensing Versus Segmented Cine Cardiac Magnetic Resonance to Assess Left Ventricular Volume and Strain1the First Affiliated Hospital of Nanjing Medical University, Nanjing, China, 2Siemens Healthineers Ltd, Shanghai, China
Synopsis
Although segmented cine cardiac magnetic resonance (CMR) is the standard choice for assessing left ventricular (LV) volume, single-shot compressed sensing (CS) cine CMR can provide similar information with shorter examination times. A total of 37 healthy patients underwent both single-shot CS and standard segmented cine imaging. The single-shot CS global strain and standard deviation of the time to peak strain were poorly to moderately correlated with those of the standard segmented cine. Inter- and intraobserver variability for LV strain were mostly good to excellent for both groups.
Introduction
Segmented cine cardiac magnetic resonance (CMR) is the standard choice for assessing left ventricular (LV) volume, although it is a time-consuming process, and image quality can be impaired by poor breath-holding or cardiac arrhythmia. Single-shot compressed sensing (CS), a new accelerated CMR technique, can accurately evaluate LV volume with significantly shorter examination times 1. LV volumetric parameters are related to LV global function, rather than regional myocardial function. Strain represents as myocardial deformation and can reflect LV regional function 2. However, strain values are various and affected by multiple factors. The acquisition modes of single-shot CS and segmented cine CMR are different, and the image quality of single-shot CS cine is slightly worse. This study aimed to assess accuracy of LV volume and strain between single-shot CS and segmented cine CMR.Methods
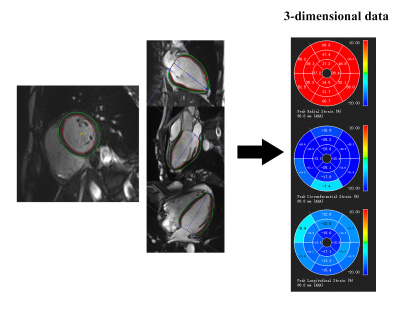
Thirty-seven healthy patients underwent single-shot CS and standard segmented cine imaging covering the whole left ventricle using a clinical 3T MR scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). To eliminate other influences to image quality, the spatial and temporal resolutions (1.7*1.7mm2 and 41ms, respectively) and other imaging parameters were set the same in the two cines. LV volumetric and strain values were analyzed by the dedicated software package (cvi42 v. 5.0, Circle Cardiovascular Imaging, Calgary, Canada;).LV volumes comprised end-diastolic volume, end-systolic volume (ESV), stroke volume (SV), ejection fraction (EF), and myocardial mass. LV endocardial and epicardial borders were traced manually on the end-diastolic phase in all short-axis and three long-axis slices, propagating the borders to subsequent phases (Figure 1). Global radial, circumferential, and longitudinal strain (GRS, GCS and GLS, respectively) were recorded. Standard deviation of segmental time to peak strain (SD-TPS) in radial, circumferential, and longitudinal three directions were obtained, which reflect cardiac mechanical desynchrony 3. All LV parameters were assessed independently by two radiologists.
Results
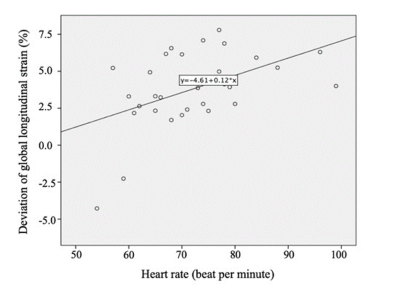
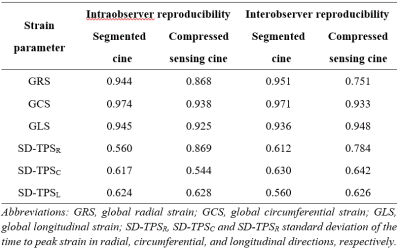
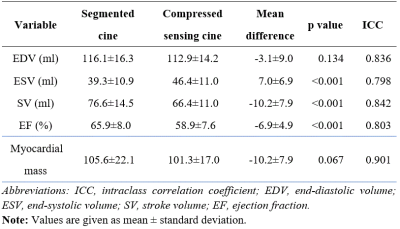
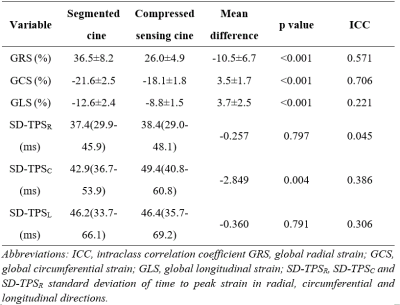
The acquisition duration was about 120s for segmented cine imaging and considerably shorter for single-shot CS cine imaging (20s). Inter‐ and intraobserver variability for LV strain from single-shot CS and segmented cine images were mostly good to excellent (Table 1).Single-shot CS cine–derived LV volumes and myocardial mass were strongly correlated with segmented cine (intraclass correlation coefficient [ICC] ≥ 0.798), although with some minor systematic overestimation of ESV leading to underestimation of EF (Table 2). Single-shot CS cine derived global strains were positively correlated with segmented cine acquisitions (ICC=0.571 and 0.706 for GRS and GCS; respectively) except for GLS (ICC=0.221). Single-shot CS cines–derived SD-TPS in three directions were poorly correlated with segmented cine imaging (ICC: 0.045-0.386). Compared with the standard of reference, global strain values were all underestimated, but no significant differences of SD-TPS in radial and longitudinal directions by single-shot CS cines were obtained (Table 3). Among the patient-related factors, only increased heart rate was consistently positively associated with underestimation of GLS (beta: 0.12% per bpm, p=0.039) after being adjusted for patient sex, age, height, weight, body mass index, and body surface area (Figure 2).
Discussion
In this study, LV volume and mass from single-shot CS cine images were strongly correlated with those of segmented cine images, with moderate to minor differences. A low but statistically significant overestimation of ESV resulted in an underestimation of SV and EF, which may be due to lower signal-to-noise ratio of single-shot CS cine images.Single-shot CS cine CMR derived global strain values were significantly lower than those from segmented cine CMR, and global strain values between both cines were not interchangeable. This finding could be explained by the variability in strain measurements among software 4, and the data acquisition and image reconstruction of single-shot CS techniques were different from those of segmented techniques. Moreover, underestimation of all global strains was found for single-shot CS cine images and deviation of GLS was primarily dependent on heart rate.
Global strain in three directions obtained by different commercial software has shown reliable reproducibility on segmented cine CMR 4, 5. Single-shot CS cine images also provided acceptable reproducibility for global strain analysis. Lower reproducibility of GRS may be partly explained by the difficulty in identifying the variation on the small distance between LV endo- and epicardium, especially on single-shot CS cine images. Another explanation could be the analysis of cardiac geometry in a plane of motion using the smallest potential diameter for tracking 6.
GLS from conventional segmented cine CMR was significantly underestimated compared with that of previous studies 7, which may be caused by different ethnicities in study population. The population of previous studies were white, whereas our study patients were Chinese. Additionally, previous studies traditionally achieved two-dimensional results for analysis of LV myocardial strain whereas our study obtained three-dimensional strain values, and LV global strain from three-dimensional CMR were lower than those from two-dimensional CMR 8.
Conclusions
Single-shot CS cine CMR is an option for assessment of left ventricular function in addition to standard segmented cine CMR. Strain values derived from the two techniques are not currently interchangeable.Acknowledgements
noneReferences
1. Kramer CM, Barkhausen J, Bucciarelli-Ducci C, et al. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson. 2020; 22 (1): 17.
2. Amzulescu MS, De Craene M, Langet H, et al. Myocardial strain imaging: review of general principles, validation, and sources of discrepancies. Eur Heart J Cardiovasc Imaging. 2019; 20 (6): 605-19.
3. Miyazaki C, Lin G, Powell BD, et al. Strain dyssynchrony index correlates with improvement in left ventricular volume after cardiac resynchronization therapy better than tissue velocity dyssynchrony indexes. Circ Cardiovasc Imaging. 2008; 1 (1): 14-22.
4. Barreiro-Perez M, Curione D, Symons R, et al. Left ventricular global myocardial strain assessment comparing the reproducibility of four commercially available CMR-feature tracking algorithms. Eur Radiol. 2018; 28 (12): 5137-47.
5. Schmidt B, Dick A, Treutlein M, et al. Intra- and inter-observer reproducibility of global and regional magnetic resonance feature tracking derived strain parameters of the left and right ventricle. Eur J Radiol. 2017; 89: 97-105.
6. Hor KN, Baumann R, Pedrizzetti G, et al. Magnetic Resonance Derived Myocardial Strain Assessment Using Feature Tracking. Journal of Visualized Experiments. 2011; (48).
7. Taylor RJ, Moody WE, Umar F, et al. Myocardial strain measurement with feature-tracking cardiovascular magnetic resonance: normal values. Eur Heart J Cardiovasc Imaging. 2015; 16 (8): 871-81.
8. Liu B, Dardeer AM, Moody WE, et al. Reference ranges for three-dimensional feature tracking cardiac magnetic resonance: comparison with two-dimensional methodology and relevance of age and gender. Int J Cardiovasc Imaging. 2018; 34 (5): 761-75.
Figures