0974
The value of CMR Feature Tracking in the differential diagnosis of isolated left ventricular noncompaction and dilated cardiomyopathy1Shanxi Cardiovascular Hospital, Taiyuan, China, 2GE Healthcare, MR Research, Beijing, China
Synopsis
In this study, myocardial strain parameters was used to distinguish Isolated left ventricular noncompaction (ILVNC) and dilated cardiomyopathy (DCM). The results showed that the apex longitudinal strain (LS) had great potential in the differential diagnosis of ILVNC and DCM, and different change patterns are presented in the LS of the myocardium from the basal segment to the apex.
Introduction
Isolated left ventricular noncompaction (ILVNC) and dilated cardiomyopathy (DCM) have signs of excessive trabecularization of the left ventricular myocardium, which brings many difficulties to clinical diagnosis and differential diagnosis1. Cardiac Magnetic Resonance Feature Tracking (CMR-FT) can evaluate myocardial strain in different directions to quantitatively assess myocardial movement2. The aim of this study is to explore the value of CMR-FT in the differential diagnosis of ILVNC and DCM.Methods
Retrospective analysis was performed on twenty-five ILVNC patients, thirty DCM patients and thirty control groups confirmed by clinical criteria and MRI. The radial strain (RS), circumferential strain (CS), and longitudinal strain (LS) of the global left ventricle and each level were measured by using CVI42 software. The comparisons of strains between groups and between different levels in the same group were conducted using analysis of variance (ANOVA). When there were significant differences in the comparison, further pairwise multiple comparisons were performed. The performance of distinguishing ILVNC and DCM through different parameters was assessed by using the receiver operating characteristic curve (ROC).Results and Discussion
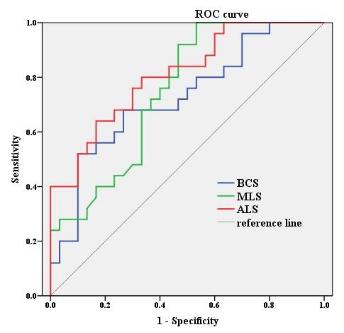
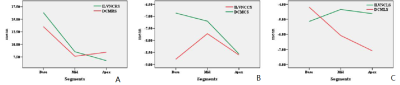
The overall and each level of RS, CS and LS of patient group were lower than those of the control group (P=0.00). The basal segment CS of the ILVNC group was higher than that of the DCM group (P=0.047), and the LS of middle(P=0.021) and apex(P=0.006 ) segments of the ILVNC group were lower than those of DCM group (Table 1). Some previous studies3,4 on myocardial strain have also shown that even in LVNC patients with normal ejection fraction, their myocardial strain has subclinical changes. The reason may be that the pathophysiological basis of LVNC is the hypertrophy and disorder of myocardial fibers in the non-compact layer of the subendocardium, leading to dysplasia of the ventricular torsion contraction system, which affects the systolic function of ventricle. The DCM is a kind of disease which is damaged outside the middle myocardium. The most significant difference between the two is the inner myocardium, and LS is caused by the longitudinally arranged myocardial fiber thickening movement in the subendocardial inner layer of the left ventricle5. Due to the increase in heart volume and decreased systolic function in DCM, excessive trabecularization of the left ventricular myocardium will be compensatory, which can increase the stroke volume by increasing the surface area of the endocardium6. This may be the reason why the LS in the ILVNC group was lower than that in DCM group. CS is mainly related to the middle myocardium. The middle myocardium of DCM is damaged, so CS is lower than that of ILVNC group. The area under the ROC curve(Fig.1) of the basal CS, middle LS, apex LS were 0.727, 0.747, 0.809, respectively, indicating that apex LS has the best performance in distinguishing ILVNC and DCM. Comparing each level of strain in the same group, the change pattern of DCM LS was different from that of ILVNC (Fig. 2).Conclusion
The parameters of myocardial strain can effectively differentiate ILVNC from DCM, which can be used as potential indicator for early clinical diagnosis.Acknowledgements
No acknowledgement found.References
1 Cortes M, Oliva MR, Orejas M, et al. Usefulness of speckle myocardial imaging modalities for differential diagnosis of left ventricular non-compaction of the myocardium. Int J Cardiol. 2016. 223: 813-818.
2 Amzulescu MS, De Craene M, Langet H. Myocardial strain imaging: review of general principles, validation, and sources of discrepancies. Eur Heart J Cardiovasc Imaging, 2019, 20(6): 605-619.
3 Finsterer J, Zarrouk-Mahjoub S. Genetic testing is not required for diagnosing leftventricular hypertrabeculation/noncompaction. Maedica, 2015, 10(1): 69-72.
4 Bellavia D, Michelena HI, Martinez M, et al. Speckle myocardial imaging modalities for early detection of myocardial impairment in isolated left ventricular noncompaction. Heart, 2010, 96(6): 440-447.
5 Tarando F, Coisne D, Galli E, et al. Left ventricular noncompaction and idiopathic dilated cardiomyopathy: The significant diagnostic value of longitudinal strain. The international journal of cardiovascular imaging, 2017, 33(1): 83-95.
6 Kawel-Boehm N, Mcclelland RL, Zemrak F, et al. Hypertrabeculated Left ventricular myocardium in relationship to myocardial function and fibrosis: the multi-ethnic study of atherosclerosis. Radiology, 2017, 284(3): 667-675.
Figures
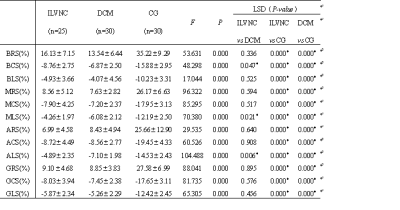
Table 1 Comparison of myocardial strain parameters in ILVNV group, DCM group and control group
The myocardial strain parameters are presented as mean±standard deviation; *P <0.05 demonstrates that the difference is statistically significant. ILVNC: Isolated left ventricular noncompaction, DCM: dilated cardiomyopathy, CG: control group, RS: radial strain, CS: circumferential strain, LS: longitudinal strain, B: Base, M: Mid, A: Apex.