0970
Myocardial Strain in Left Atrium in Smoking Population with Magnetic Resonance Imaging: A Pilot Study1The First Affiliated Hospital of Dalian Medical University, Dalian, China, Dalian, China
Synopsis
The purpose of this study is to explore the correlation between smokers' left atrium (LA) myocardial strain (MS), total ejection fraction (EFtotal) parameters and smoking parameters. This study demonstrated that LA global longitudinal strain (GLS) was significantly impaired and reduced with prolonged duration of smoking, smoking intensity and smoking burden.
Main findings
With the increase of smoking time, smoking intensity and smoking burden, LA GLS were significantly impaired and decreased.Introduction
According to the World Health Organization (WHO) data in 2017, as of 2016, the number of tobacco users worldwide reached 1.3 billion, and more than 6 million people died directly or indirectly from tobacco smoke damage each year [1]. Many studies have confirmed the effects of acute or chronic smoking on myocardial contractile, diastolic properties. At present, related studies have clearly stated that smoking is not only the most common risk factor for COPD, but also an independent risk factor for COPD-related pulmonary hypertension (PH). Smoking is also a risk related to lung cancer, stroke, and cardiovascular disease [2-4].In addition, IlgenliTF et al.[5] conducted a comparative study of 20 healthy young male volunteers who completed the echocardiographic examination results before and after smoking and found that the ratio of the peak filling velocity of the tricuspid valve at the end of diastole to the early diastole of the right ventricle (RV) decreased significantly at 5 and 15 minutes, proving that smoking impaired the diastolic function of RV in the acute phase. However, few researchers have used cardiac magnetic resonance imaging (CMR) to evaluate the effect of chronic smoking on LA. The purpose of this study is to explore the correlation between smokers' LA MS, EFtotal parameters and smoking parameters, to provide a theoretical basis for in-depth understanding of the effects of smoking on the left atrium.
Materials and methods
36 healthy male volunteers (mean age: 47.22 ± 11.49, range: 25-68 years) with different degrees of smoking history who underwent cardiac 3.0T MRI (HDxt; General Electric Medical Systems, Waukesha, WI, USA) examinations at the First Affiliated Hospital of Dalian Medical University from May 2019 to January 2020 were included in the study. Scanning parameters included: TR/TE = 3.6/1.6ms, flip angle = 50°, FOV = 350×350 mm2, matrix size = 192×224, slice thickness = 10 mm, and slice gap = 0 mm. A questionnaire survey was used to record and summarize the detailed smoking status of each volunteer. Using fast imaging employing steady state acquisition (FIESTA) cine sequence imaging, regular scanning levels mainly included the long axis of the left ventricle, the inflow and outflow tract, the four-chamber heart, and the short axis of the left ventricle (from the apex to the base) film images. GLS, global circumferential strain (GCS), global radial strain (GRS) in LA and other parameters assessed by Medis Suite (Medis Medical Imaging Systems, Leiden, the Netherlands). The correlation analysis between smoking parameters and LA MS was completed by SPSS 22.0 (Chicago, IL, USA) software.Result
Smoking time, smoking intensity and smoking burden was a negatively correlated with LA GLS, respectively (r =-0.383,p =0.021;r =-0.423,p =0.010;r =-0.399,p =0.016). However, there was no a correlation in LA GCS, GRS, LAEF and smoking parameters (p >0.05).Conclusion
With the increase of smoking time, smoking intensity and smoking burden, LA GLS are significantly impaired and decreased.Acknowledgements
no acknowledgementReferences
[1] Organization WH.WHO report on the global tobacco epidemic 2017: Monitoring tobacco use and prevention policies.2017
[2] Sharma A, Bansal-Travers M, Celestino P, Fine J, Reid ME, Hyland A, et al.Using a Smoking Cessation Quitline to Promote Lung Cancer Screening. Am J Health Behav. 2018 Nov 1;42(6):85-100.
[3] Kundu S, Ramshankar V, Verma AK, Thangaraj SV, Krishnamurthy A, Kumar R,et al. Association of DFNA5, SYK, and NELL1 variants along with HPV infection in oral cancer among the prolonged tobacco-chewers. Tumour Biol. 2018 Aug;40(8):1010428318793023.
[4] Ding N, Sang Y, Chen J, Ballew SH, Kalbaugh CA, Salameh MJ, et al. Cigarette Smoking, Smoking Cessation, and Long-Term Risk of 3 Major Atherosclerotic Diseases. J Am Coll Cardiol. 2019 Jul 30;74(4):498-507.
[5] Ilgenli TF, Akpinar O. Acute effects of smoking on right ventricular function. A tissue Doppler imaging study on healthy subjects. Swiss Med Wkly. 2007 Feb 10;137(5-6):91-6.
Figures
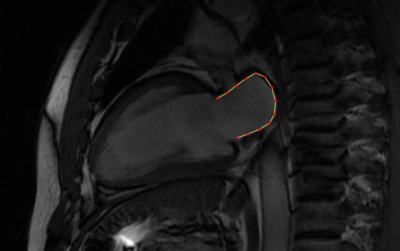
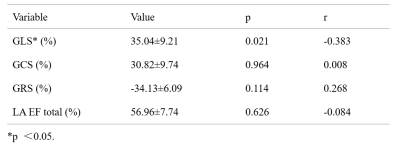
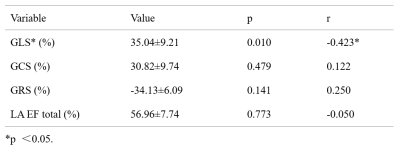
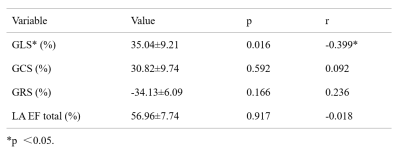
Table 3: Correlation analysis between smoking burden and LA MS in male smokers