0876
Functional Reorganization associated with Language Recovery after Repetitive Transcranial Magnetic Stimulation in Chronic Aphasic Stroke1Biomedical Imaging and Radiological Sciences, National Yang Ming University, Taipei, Taiwan, 2Physical Medicine and Rehabilitation, Taipei Veterans General Hospital, Taipei, Taiwan
Synopsis
Low-frequency repetitive transcranial magnetic stimulation (rTMS) provided promising results to facilitate the language recovery in stroke patients with non-fluent aphasia. This study demonstrated that the contralesional inhibitory rTMS treatment can induce the functional reorganization within language networks and recovery of language function in chronic aphasic stroke. The correlation analysis further revealed the association between altered functional connectivity and improved language ability after rTMS treatment. Finally, we reported that the involved functional circuits for the language recovery may depend on lesion location and size of stroke.
Background and Purpose
Aphasia is most often caused by either ischemic or hemorrhagic stroke when the brain language areas, such as the left inferior frontal gyrus, left superior temporal gyrus and the basal ganglia, are damaged. During the past decade, several studies showed that the low-frequency repetitive transcranial magnetic stimulation (rTMS) applied over the contralesional pars triangularis could induce an inhibitory effect to downregulate the circuits in normal hemisphere and hence benefits the language recovery.1 Although rTMS exhibited promising efficacy in treating aphasic stroke, the underlying neuroplastic process (functional reorganization) induced by rTMS remains inconclusive.2 We anticipated that functional circuits related to language recovery in each patient may depend on the lesion location, size, and distribution after the rTMS treatment.Materials and Methods
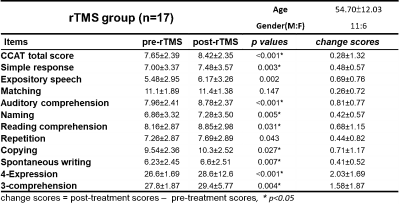
This study was approved by the local Institutional Review Board, and the written informed consent was provided by each participant. Seventeen patients with chronic stroke (at least 3 months after stroke) located in left hemisphere and diagnosed as non-fluent aphasia were recruited. The enrolled patients were treated with 1 Hz-rTMS on the contralesional pars triangularis for 10 daily sessions. All the patients received language therapy twice a week. The Concise Chinese Aphasia Test (CCAT) with nine testing items, including simple response, expository speech, matching, auditory comprehension, naming, reading comprehension, repetition, copying, spontaneous writing, was used to assess the language functions.3 Three more composite scores, including 4-expression (calculated as the sum score of simple response, expository speech, naming, and copying), 3-comprehension (calculated as the sum score of matching, auditory comprehension, and reading comprehension) and total scores were also evaluated. MRI data, including a 3D-FSPGR T1-weighted images (TR/TE: 9.4/4.0 ms; voxel size: 1.0x1.0x1.0 mm3) and BOLD resting-state fMRI (TR/TE: 2500/30 ms; voxel size: 3.5x3.5x3.5 mm3, 190 volumes) were acquired on a 3T MR scanner (GE Discovery MR750). Each patient received twice MRI scans before and after the treatment to evaluate the changes of brain functional networks. The fMRI data were preprocessed using SPM12 with the standard procedures: correction for slice timing, realigned, co-registration with structural images, spatially normalization into the MNI standard space, and spatially smoothing with a 6-mm FWHM Gaussian kernel.4 The selected regions related to language network included the inferior frontal gyrus (pars opercularis, triangularis and orbitalis), angular gyrus, superior temporal gyrus, putamen, caudate, thalamus, anterior cingulated gyrus, insula, precentral gyrus, postcentral gyrus and cerebellum within both hemispheres. The functional connectivity (FC) between the selected regions was calculated using the Pearson’s correlation coefficient.5,6,7 Most of the mean BOLD signals were extracted using a 6-mm sphere from the center of each selected cortex, while mean signals of putamen, caudate, thalamus was extracted based on the AAL 116 template.The correlation analysis between CCAT and FC were performed to identify high correlation circuits (|r|>0.65, p<0.05). Finally, hierarchical clustering (HC) was performed to cluster all the patients into four groups (aphasia subtypes) based on the individual lesion pattern and to identify associated functional circuits for language recovery after rTMS.
Results and Discussion
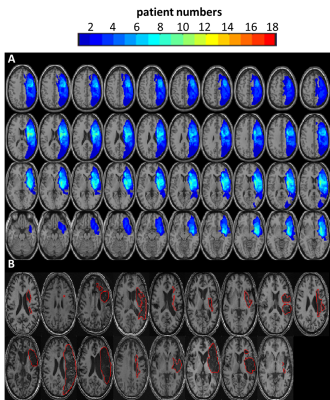
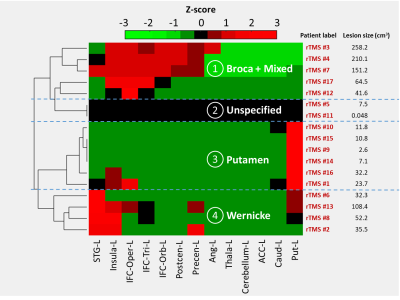
Table 1 lists the changes of language performance (each item of CCAT, 4-expression, 3-comprehension and total scores) before and after rTMS treatment. The recruited patients with rTMS treatment showed significant improvement (positive values of change score, p<0.05) of the total scores along with the items of simple response, auditory comprehension, naming, reading comprehension, copying, spontaneous writing, 4-expression and 3-comprehension. Our results are consistent with previous studies that rTMS treatment can improve the language performance.1,8 Figure 1A shows that the distribution maps of stroke lesions among 17 recruited patients, and Figure 1B demonstrates that the lesion pattern of each patient. It was obvious that the lesion location and size of patients were diverse, and therefore we applied HC and correlation analysis to investigate whether distinct alterations of FC (for different aphasia subtypes) may be involved to facilitate the language recovery after rTMS. Figure 2 shows all the patients were clustered into four aphasia subtypes with stroke lesion mainly involved in Broca and mixed type (sensorimotor and insula), unspecified, putamen and Wernicke areas.Figure 3a and 3b demonstrate the FC between left pars triangularis and superior temporal gyrus positively correlated with total scores and 4 expression. In addition, the patients classified as the putamen and unspecified subtypes, whose lesion did not involve the Broca or Wernicke areas, tended to have better language performance as this FC maintained. Figure 3c to 3f show positive correlations between FCs and language functions. It is noted that data from patients with lesion outside the areas related to the specified FC distribute along the fitted correlation lines, indicating the distinct reorganized circuits and responses to the rTMS treatment between patients. Figure 3g shows that the FC between left pars triangularis and right superior temporal gyrus is negatively correlated with auditory comprehension, which implies that the enhancement of FC across hemispheres after stroke may impede the language recovery.
Conclusions
This study reported the efficacy of rTMS for improving language functions and inducing functional reorganization in patients with chronic aphasic stroke. By combining HC and correlation analysis, we proposed that the individual lesion pattern (location and size) may be a key factor to determine the functional circuits related to the language improvement after the inhibitory rTMS treatment.Acknowledgements
This work was supported by the Ministry of Science and Technology, Taiwan (MOST 109-2314-B-010-022-MY3) and the National Yang-Ming University (VGHUST110-G7-2-2).
References
1. Naeser, M.A., et al., Research with rTMS in the treatment of aphasia. Restor Neurol Neurosci, 2010. 28: p. 511-529.
2. Turkeltaub, Peter E., et al. "Are networks for residual language function and recovery consistent across aphasic patients?." Neurology 76.20 (2011): 1726-1734.
3. Chung, Y.M., et al., The Concise Chinese Aphasia Test (CCAT) and it's application. The journal of Speech-language-hearing association, 1998. 13: p. 119-137.
4. Penny WD, Friston KJ, Ashburner JT, Kiebel SJ, Nichols TE, editors. Statistical parametric mapping: the analysis of functional brain images. Elsevier; 2011 Apr 28.
5. Crosson, B., et al., Functional imaging and related techniques: an introduction for rehabilitation researchers. Journal of rehabilitation research and development, 2010. 47(2): p. vii.
6. Branco, P., et al., Resting-state functional magnetic resonance imaging for language preoperative planning. Frontiers in human neuroscience, 2016. 10: p. 11.
7. Petrides, M., Neuroanatomy of language regions of the human brain. 2013: Academic Press.
8. Harvey, Denise Y., et al. "Functional reorganization of right prefrontal cortex underlies sustained naming improvements in chronic aphasia via repetitive transcranial magnetic stimulation." Cognitive and behavioral neurology: official journal of the Society for Behavioral and Cognitive Neurology 30.4 (2017): 133.
Figures