0858
An Anthropomorphic Pelvis Phantom for Prostate Brachytherapy and Biopsy1Computer Assisted Clinical Medicine, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany, 2Mannheim Institute for Intelligent Systems in Medicine, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany, 3Fraunhofer Institute for Manufacturing Engineering and Automation, Project Group for Automation in Medicine and Biotechnology, Mannheim, Germany, 4Department of Radiology and Nuclear Medicine, University Medical Center Mannheim, Mannheim, Germany, 5Department of Radiation Oncology, University Medical Center Mannheim, Heidelberg University, Mannheim, Germany
Synopsis
We present an anthropomorphic pelvis phantom with lesions for transperineal and transrectal prostate needle interventions. The human-sized artificial pelvis includes bones, bladder, prostate with four lesions, urethra, arteries, veins and six lymph nodes embedded in ballistic gelatin. It is puncturable and shows realistic contrast in multiparametric MRI (mpMRI) as well as CT imaging. The phantom can be used for the evaluation, training and finetuning of multimodal prostatic intervention procedures, such as prostate brachytherapy and biopsy.
Introduction
Multiparametric MRI (mpMRI) is of high value for the detection and characterization of prostate cancer1. Anatomic sequences allow for the morphologic evaluation of the prostate tissue. Complementary functional sequences with diffusion and perfusion techniques are used to assess prostatic lesions and local tumor staging2. MpMRI can be applied for prostate cancer management and therapy planning in order to identify clinically significant cancer and to localize index lesions3,4. Accurate localization of the index lesion enables targeted biopsies and optimized radiation dose planning for brachytherapy5,6. Prostate brachytherapy and prostate biopsy are commonly conducted in interventional CT. At our university hospital, a hybrid interventional suite (iMRI suite) was established comprising an MRI and an interventional CT device. Patients are positioned on an innovative CT- and MR-suited couch which can be transferred between the imaging modalities without dismounting the patient.Preliminary validation using imaging phantoms is a vital step for the introduction of new technologies like robotic needle guidance into the clinical routine. However, established pelvis and prostate phantoms in literature are either not anthropomorphic or not puncturable7,8. We present an anthropomorphic pelvis phantom for transperineal and transrectal prostate needle interventions. The phantom is puncturable and suitable for MR and CT imaging. The phantom is reusable, since the puncture channels can be easily removed in a simple remolding step.
Methods
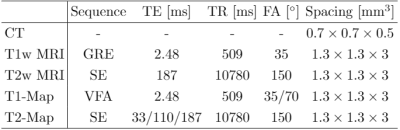
The phantom components were manufactured with several 3D printing techniques as well as molding of silicone and ballistic gelatin. Except for the bladder and prostate, all organ 3D models illustrated in Fig. 1 (a) were obtained from segmentations of the digital XCAT phantom9. The bones were 3D printed via selective laser sintering (SLS) using polyamide powder filled with glass particles. The material exhibits excellent stiffness, high density, high thermal resistance and tensile strength. The inside of the bones is printed less densely to simulate bone marrow. The artery and vein were printed with red and blue High Impact Polystyrene (HIPS) via Fused Filament Fabrication (FFF). The bladder and prostate were molded with silicones of shore hardness 0 and 5, respectively (Fig. 2 (b), (c)). A silicone of shore hardness 13 was used for the prostate lesions and lymph nodes. The diameter of the spherical prostate lesions is 1.2cm and 1.5-2cm for the lymph nodes. The rectum is hollow which allows for a transrectal access of the prostate. The urethra and body casting mold were printed via stereolithography (SLA) with a heat resistant high temp resin. The casting mold of the body was designed in 16 parts which were screwed together and sealed with high temperature silicone. The organs were glued together as shown in Fig. 1 (b) and placed inside the body casting mold shown in Fig. 2 (a). Ballistic gelatin was melted in an oven at 140°C and poured into the body hull.3 Tesla MRI and CT scans of the phantom were acquired with MAGNETOM Skyra and SOMATOM Force scanners (Siemens Healthineers, Germany), respectively. The scanning parameters are listed in Table 1.
Results
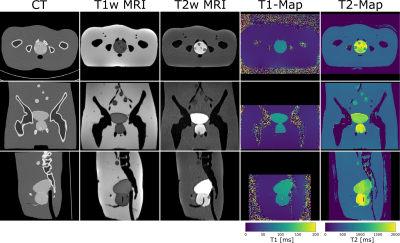
The manufactured phantom is pictured in Fig. 1 (c). In Fig. 3 a CT scan, T1w and T2w MRI scans and T1- and T2-Maps are shown. Except for arteries and veins all organs are clearly distinguishable in the CT scan. The prostate lesions are well detectable in T2w MRI and not visible in T1w MRI. This observation is supported by the quantified T1- and T2-Maps. In comparison to the prostate material, the prostatic lesions show noticable differences in rigidity.Discussion
Our results demonstrate that the artificial pelvis shows human-like contrast in several MRI sequences as well as CT. The size of the presented 30cm tall phantom is comparable to a real human pelvis. This allows the evaluation and optimization of the complete workflow from patient positioning to multimodal imaging protocols and finally intervention.The high visibility of the prostate lesions in CT and MRI scans of the phantom in combination with the hollow rectum is central for seed application and other prostate interventions. Prostatic lesions simulate realistic haptic feedback during needle insertion, which is essential to train surgical personnel. The included bladder and urethra serve as realistic inhibitions for needle-based intervention planning. The lymph nodes act as additional percutaneous needle targets, with blood vessels as risk structures.
The multimodal properties of the phantom enable the verification of MR-based radiotherapy treatment planning methods. Currently, CT images are the basis of dose calculations in treatment planning. A crucial step towards MR-only radiotherapy treatment planning is accurate MR-to-CT synthesis10, for which this phantom provides co-registered ground truth data.
Conclusion
We designed and manufactured a multimodal pelvis phantom. It can be punctured and exhibits realistic imaging characteristics. The phantom can be used to evaluate, practice and finetune multimodal transperineal and transrectal prostatic intervention procedures in a novel iMRI suite.Acknowledgements
This research project is part of the Research Campus M2OLIE and funded by the German Federal Ministry of Education and Research (BMBF) within the Framework "Forschungscampus: public-private partnership for Innovations" under the funding code 13GW0388A.References
1. Dickinson, L., et al. "Magnetic resonance imaging for the detection, localisation, and characterisation of prostate cancer: recommendations from a European consensus meeting." European urology 59.4 (2011): 477-494.
2. Stabile, A., et al. "Multiparametric MRI for prostate cancer diagnosis: current status and future directions." Nature reviews urology 17.1 (2020): 41-61.
3. Radtke, J. P., et al. "Multiparametric magnetic resonance imaging (MRI) and MRI–transrectal ultrasound fusion biopsy for index tumor detection: correlation with radical prostatectomy specimen." European urology 70.5 (2016): 846-853.
4. Le, J. D., et al. "Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology." European urology 67.3 (2015): 569-576.
5. Noureldin, M., et al. "MRI-targeted biopsies for prostate cancer diagnosis and management." World Journal of Urology (2020): 1-7.
6. Wang, J., et al. "Magnetic resonance imaging basics for the prostate brachytherapist." Brachytherapy 16.4 (2017): 715-727.
7. Chiu, T., et al. "Low-cost 3D print–based phantom fabrication to facilitate interstitial prostate brachytherapy training program." Brachytherapy (2020).
8. Niebuhr, N. I., et al. "The ADAM-pelvis phantom—an anthropomorphic, deformable and multimodal phantom for MRgRT." Physics in Medicine & Biology 64.4 (2019): 04NT05.
9. Segars, W. P., et al. "4D XCAT phantom for multimodality imaging research." Medical physics 37.9 (2010): 4902-4915.
10. Wolterink, J. M., et al. "Deep MR to CT synthesis using unpaired data." International workshop on simulation and synthesis in medical imaging. Springer, Cham, 2017.
Figures


Figure 2: (a) Body casting mold. (b) Prostate casting mold including prostate lesions and urethra. The lesions and urethra were placed inside the mold before molding. (c) Bladder and Bladder casting mold.