0844
Analysis of Diffusion Changes in Patients with Juvenile Osteochondritis Dissecans (JOCD) of the Knee at 3T1Center for Magnetic Resonance Research, University of Minnesota, Minneapolis, MN, United States, 2Research Unit of Medical Imaging, Physics and Technology, University of Oulu, Oulu, Finland, 3Department of Radiology, University of Minnesota, Minneapolis, MN, United States, 4Department of Veterinary Clinical Sciences, University of Minnesota, Minneapolis, MN, United States, 5Department of Orthopaedic Surgery, University of Minnesota, Minneapolis, MN, United States
Synopsis
This 3T study evaluates 46 juvenile osteochondritis dissecans (JOCD) lesions of 41 skeletally immature patients using clinical, morphological MRI and diffusion-weighted MRI (DWI). In this study, apparent diffusion coefficient (ADC) values were able to differentiate between healed and not yet healed JOCD lesions, and distinguish between the operative and nonoperative treatment groups. DWI provides noninvasive, quantitative assessment of disease status which may help inform clinical management of JOCD. Further follow-up studies are needed to evaluate the potential of DWI for the prediction of lesion healing in JOCD patients.
PURPOSE
Juvenile osteochondritis dissecans (JOCD) is a skeletal disorder affecting epiphyseal (growth) cartilage and adjacent subchondral bone of the distal femur in children1. Clinical management of patients with stable lesions usually includes nonoperative therapy for 6-12 months, which is unsuccessful in about 50% of patients that subsequently require surgical treatment2. Unfortunately, predictors such as age, lesion size, or presence of cysts do not allow reliable prediction of treatment outcome2. Diffusion-weighted MRI (DWI) is sensitive to molecular motion of water protons and thus enables non-invasive evaluation of tissue microstructure. Previous DWI studies detected higher apparent diffusion coefficient (ADC) values in post-traumatic bone marrow than in normal bone marrow3,4. This study: (i) investigates ADC values within the JOCD lesions, surrounding bone marrow, and adjacent cartilage; (ii) compares ADC values between different stages of the disease; and (iii) evaluates ADC values in patients that receive operative treatment vs. patients that are free of symptoms after nonoperative treatment.METHODS
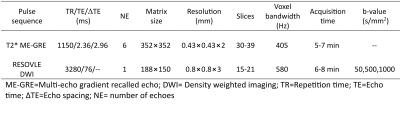
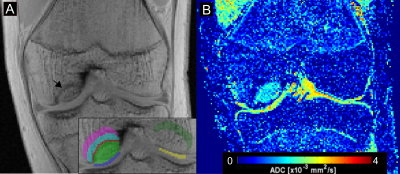
Forty-one patients (24 males; average age = 12.8 years; range = 8-19 years) with 46 JOCD lesions were enrolled in this study approved by the institutional review board. All images were acquired at 3T MRI system (Siemens, Erlangen, Germany) with a 1Tx/15Rx knee coil (Quality Electrodynamics, Mayfield Village, OH). Morphological T1-weighted, T2-weighted, and PD-weighted images were collected for evaluation of lesion stability. A multi-echo T2* mapping sequence and a segmented, multi-shot DWI sequence with fat suppression were acquired (Figure 1). Using a previously described lesion staging system1, each lesion was assigned a stage reflecting the natural history of JOCD. DWI images were initially denoised using the MPPCA method5 and then co-registered to the first echo of T2*-weighted images. ADC maps were calculated from DWI images using a mono-exponential least-square fitting algorithm. Seven regions of interest (ROIs) were drawn within each JOCD-affected knee on the first echo T2* images using ITK-SNAP. Five regions were selected in the femoral condyle with the lesion (progeny lesion, interface, adjacent parent bone, distant parent bone and adjacent cartilage) and two regions on the opposite, healthy condyle (contralateral parent bone and contralateral cartilage) (Figure 2). The ROIs were transferred to the coregistered ADC maps and the median ADC values were calculated in each ROI. Nonparametric Mann-Whitney U tests (comparing surgical vs. non-surgical patients), Kruskal-Wallis tests (comparing patients with different JOCD stages), and Spearman correlation coefficients (ρ) were calculated for statistical evaluations.RESULTS
Forty-six JOCD lesions were classified as JOCD stage I (n=7), stage II (n=20), stage III (n=12) and stage IV (n=7). Additionally, 13 lesions (stage II or III) that received surgical treatment after MRI were compared with 9 lesions (stage II or III) from patients that lost symptoms after conservative, non-surgical treatment. Comparing regions between different JOCD stages, ADC values in the progeny lesion, interface, and adjacent parent bone were significantly lower at stage IV than at stages I-III (Figure 3). Weak to moderate negative correlations between ADC values and JOCD stage were observed in the progeny lesion (ρ=-0.515, p<0.001), adjacent parent bone (ρ=-0.421, p=0.004), interface (ρ=-0.314, p=0.034), and distant parent bone (ρ=-0.314, p=0.035) (Figure 4). The comparison between different treatment groups showed significantly higher ADC values in the interface (p=0.001), adjacent parent bone (p=0.012), distant parent bone (p=0.03), and cartilage under the lesion (p=0.012) of patients in the operative group when compared to patients in the non-surgical treatment group (Figure 5).DISCUSSION
Our results showed elevated ADC values in the progeny lesion, interface and adjacent parent bone in early stages of JOCD (stages I-III) when compared to the healed, stage IV JOCD lesions. However, the ADC values in these regions at stage IV were not significantly different from values in the normal, contralateral parent bone. A decrease of ADC values in the lesion and surrounding tissues during the disease progression can be explained by the gradual ossification of the lesion area that restricts water diffusion1. Elevated ADC values were previously reported in bone marrow after knee trauma, where injured bone marrow went through the repair process of disrupted trabeculae3,4. Initially increased ADC values in JOCD lesions and the surrounding parent bone might therefore indicate abnormal composition of bone marrow and/or undergoing tissue repair that normalizes at a later disease stage when the lesion heals. We also observed higher ADC values in the interface and parent bone of patients in the operative group than in the nonoperative treatment group, which might be due to different composition of the tissue created during JOCD progression. ADC values in cartilage adjacent to JOCD lesions were not significantly different between JOCD stages and were comparable to ADC in control cartilage, suggesting that JOCD does not influence the integrity of the overlying cartilage. This is in agreement with previous T2 and T2* mapping studies of cartilage in JOCD patients6,7.In conclusion, DWI enables quantitative assessment of JOCD lesions and surrounding tissues, can differentiate between healed and not yet healed JOCD lesions, and can distinguish between the operative and nonoperative treatment groups. Further follow-up studies are needed to evaluate the potential of DWI for the prediction of lesion healing and clinical management (operative versus nonoperative treatment) of JOCD patients.
Acknowledgements
This study was supported by the NIH, NIAMS grants (R01 AR070020, K01 AR070894, T32 AR050938) and NIBIB grant (P41 EB027061).References
1. Ellermann J, Johnson CP, Wang L, et al. Insights into the Epiphyseal Cartilage Origin and Subsequent Osseous Manifestation of Juvenile Osteochondritis Dissecans with a Modified Clinical MR Imaging Protocol: A Pilot Study. Radiology. 2017; 282: 798-806
2. Krause M, Hapfelmeier A, Moller M, et al., Healing predictors of stable juvenile osteochondritis dissecans knee lesions after 6 and 12 months of nonoperative treatment. Am J Sports Med. 2013; 41(10): 2384-2391.
3. Ward R. Caruthers S, Yablon C, et al. Analysis of Diffusion Changes in Posttraumatic Bone Marrow Using Navigator-Corrected Diffusion Gradients. Am J Roentgenol. 2000; 174: 731-734.
4. Klengel A, Stumpp P, Klengel S, et al. Detection of Traumatic Bone Marrow Lesions after Knee Trauma: Comparison of ADC Maps Derived from Diffusion-weighted Imaging with Standard Fat-saturated Proton Density–weighted Turbo Spin-Echo Sequences. Radiology. 2017; 283(2): 469–477.
5. Veraart J, Novikov SD, Christiaens D, et al. Denoising of diffusion MRI using random matrix theory. Neuroimage. 2016; 142: 394-406.
6. Nguyen JC, Liu F, Blankenbaker DG, et al. Juvenile Osteochondritis Dissecans: Cartilage T2 Mapping of Stable Medial Femoral Condyle Lesions. Radiology. 2018; 288(2): 536-543.
7. Ludwig KD, Johnson CP, Zbyn S, et al. MRI evaluation of articular cartilage in patients with juvenile osteochondritis dissecans (JOCD) using T2 * mapping at 3T. Osteoarthritis Cartilage 2020; 28(9): 1235-1244.
Figures