0770
Reproducibility study of disrupted white matter integrity and partial recovery in children treated for medulloblastoma1Department of Diagnostic Imaging, St. Jude Children's Research Hospital, Memphis, TN, United States, 2Department of Biostatistics, St. Jude Children's Research Hospital, Memphis, TN, United States, 3Department of Oncology, St. Jude Children's Research Hospital, Memphis, TN, United States, 4Department of Radiation Oncology, St. Jude Children's Research Hospital, Memphis, TN, United States
Synopsis
The current reproducibility study evaluates 140 children treated for medulloblastoma and 92 age-similar controls using TBSS analysis of FA and dosimetry accounting for age. Treatment included surgery, post-operative standard or high dose craniospinal irradiation and adjuvant chemotherapy. FA measures at baseline after surgery but prior to therapy demonstrated an immediate decrease due to tumor and surgery, which was then accentuated by irradiation. A partial recovery of FA followed, which was attenuated in patients receiving higher doses. These longitudinal profiles need to be considered when conducting cross-sectional studies of patients at time points during or after therapy.
INTRODUCTION:
A previous study comparing patients treated for medulloblastoma, stratified into average- and high-risk groups, and age similar controls demonstrated that patients had decreased fractional anisotropy (FA) at baseline, which then increased following therapy but not to the level of the controls.1 As a reproducibility study, we evaluated an independent cohort of patients treated for medulloblastoma and compared results with earlier findings.METHODS:
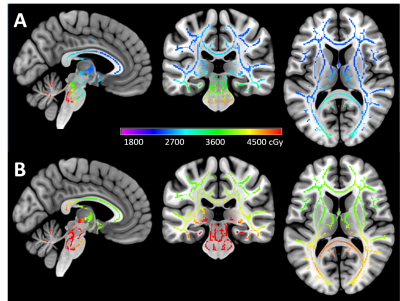
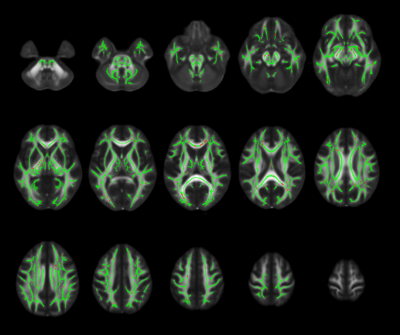
Patients (N=140) with newly diagnosed medulloblastoma were enrolled and imaged on a phase II therapeutic trial (NCT01878617) at a single institution. All patients first underwent maximal tumor resection followed by risk-adapted radiation therapy and adjuvant chemotherapy stratified by a combination of molecular and clinical factors. Patients were imaged at five time points: baseline following tumor resection, after radiation therapy, immediately after adjuvant chemotherapy, three months after adjuvant chemotherapy, and nine months after adjuvant chemotherapy. Healthy age-similar controls (N=92) underwent three MRI examinations one year apart. Treatment and imaging protocols were approved by the Institutional Review Board, and written informed consent was obtained from the patient, parent, or guardian, as appropriate for all patients and controls.All DTI were performed on a 3.0T MRI scanner (Siemens Medical Systems). For control subjects, DTI was acquired with four acquisitions and 12 directions using a double-spin echo, EPI pulse sequence (FOV, 230 mm; TR, 6500-8000 ms; TE, 120 ms; resolution, 1.8 x 1.8 x 3.0 mm with b = 700 s/mm2). Early patient DTI were acquired with two acquisitions and 30 directions using a single-shot EPI sequence (FOV, 230 mm; TR, 14000 ms; TE, 120 ms; resolution 1.8 x 1.8 x 2.0 mm; b = 700 s/mm2). Starting in 2016, acquisitions transitioned to a multi-band EPI sequence with two reverse blip acquisitions and 64 directions (FOV, 230 mm; TR, 4000 ms; TE, 77.4 ms; MB, 4; resolution 1.8 x 1.8 x 1.8 mm; b = 1500 s/mm2). Radiation dosimetry maps were generated from the therapy plans and registered to the DTI (Figure 1).
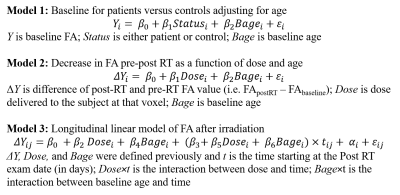
Tensor parameters were calculated for each voxel using FMRIB’s Diffusion Toolbox (FDT) from FSL and eigenvalues were combined to form FA maps.2 Voxel-wise statistical analysis of the FA maps with corresponding individualized dosimetry maps were carried out using tract-based spatial statistics (TBSS).3 A piece-wise statistical approach was used to assess: a linear regression model of baseline FA, a linear regression model of pre-post RT, and a linear mixed effects model from post-RT to end of imaging (Figure 2). First analysis assessed baseline for patients versus controls adjusting for age with Model 1. Second analysis assessed the decrease in FA pre-post RT in relation to dose or age with Model 2. Third analysis addressed the linear longitudinal evolution of the FA after irradiation. All hypotheses were tested using a likelihood ratio test.
RESULTS:
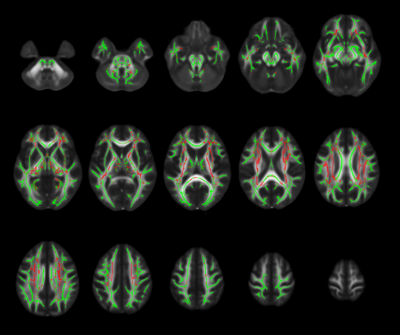
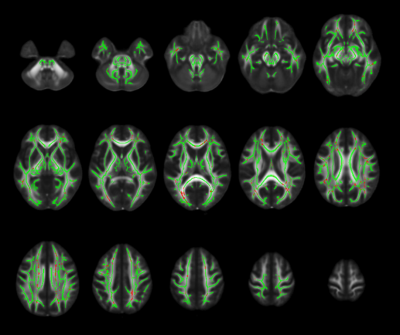
In the baseline analysis, FA significantly increased with baseline age in almost all voxels, but patients continue to have significantly lower FA than controls in 93,486 voxels (89% of all voxels tested) as shown in the previous study. The immediate changes over the radiation therapy window demonstrated a significant decrease in FA values in 21,891 (21%) of all voxels tested. Distributions of these voxels were primarily in the internal/external capsule, corpus callosum, and corona radiata including the superior longitudinal fasciculus (Figure 3). The immediate FA change was not significantly related to either dose or baseline age. The longitudinal evolution of the FA after irradiation showed that the change over time (slope) was significantly positive in 8165 (7.8%) of all voxels tested, as shown in the previous study, demonstrating a partial recovery of the FA in the period following irradiation (Figure 4). While there was no significant impact of age on the FA recovery, there was a significant negative interaction between dose and time such that higher doses attenuated the rate of recovery in a total of 3087 (2.9%) voxels. The distributions of these voxels were primarily in the cerebral peduncles, internal capsule, posterior thalamic radiation, corpus callosum, and corona radiata including the superior longitudinal fasciculus (Figure 5).DISCUSSION:
This study successfully replicated the primary findings of the previous study in an independent cohort of pediatric patients treated for medulloblastoma. Patients continue to demonstrate significantly decreased FA compared to controls at baseline due to tumor and surgery. There is a significant decrease in FA over the course of irradiation that is not related to age or dose. Patients demonstrate a significant partial recovery of FA post-irradiation; however, this recovery is attenuated in those who receive higher doses. These results are consistent with white matter volume changes observed in pre-clinical models.4 The results identified several white matter tracts that are particularly vulnerable to damage. It will be important to associate recovery of FA with neurocognitive performance in these subjects.CONCLUSION:
Compared to controls, children treated for medulloblastoma have decreased values of FA after surgery and craniospinal irradiation. Recovery of FA values after treatment is partial and attenuated by higher radiation doses. Tumor and therapy-related longitudinal changes in FA need to be considered when conducting cross-sectional studies of patients at time points during or after therapy for medulloblastoma.Acknowledgements
No acknowledgement found.References
1. Glass JO, Ogg RJ, Hyun JW, et al. Disrupted development and integrity of frontal white matter in patients treated for pediatric medulloblastoma. Neuro Oncol. 2017;19: 1408-1418.
2. Smith SM, Jenkinson M, Woolrich MW, et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23 Suppl 1: S208-219.
3. Smith SM, Jenkinson M, Johansen-Berg H, et al. Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. Neuroimage. 2006;31: 1487-1505.
4. Nieman BJ, de Guzman AE, Gazdzinski LM, et al. White and Gray Matter Abnormalities After Cranial Radiation in Children and Mice. Int J Radiat Oncol Biol Phys. 2015;93: 882-891.
Figures