0746
The Impact of Acceleration on Radiologists' Confidence in Point-Of-Care 0.5T MRI For Triage of Acute Stroke1School of Biomedical Engineering, Dalhousie University, Halifax, NS, Canada, 2Biomedical Translational Imaging Centre, QEII Health Sciences Centre, Halifax, NS, Canada, 3Physics and Atmospheric Science, Dalhousie University, Halifax, NS, Canada, 4Medicine, Dalhousie University, Halifax, NS, Canada, 5Diagnostic Radiology, Dalhousie University, Halifax, NS, Canada, 6Diagnostic Imaging, Nova Scotia Health, Halifax, NS, Canada
Synopsis
Accelerated MR image acquisition is key for emergency medicine situations, such as acute stroke, but yields degraded image quality. Therefore, our aim in this study was to calibrate a relationship between IQMs and radiologists' confidence in answering pointed clinical questions relevant to triaging of stroke patients so as to develop a protocol at low-field that is “as fast as clinically useful”. We observed that upon increasing R and decreasing NEX, radiologists’ confidence scores in their ability to identify diagnostically relevant features of both acute and chronic stroke decreased; however, radiologists’ confidence remained high despite retrospective acceleration of up to R=6.
Introduction
MRI yields superior contrast for many neurological pathologies1,2, but the time needed to fully sample k-space yields a slow acquisition process, thereby restricting the use of MR in time-sensitive applications, such as acute stroke triaging. Reducing the percentage of k-space data acquired will proportionately accelerate acquisition time but degrade image quality. However, depending on the application, this reduction in quality may not impact a radiologist’s ability to identify diagnostically relevant features.The novel, head-only, 0.5T MRI system from Synaptive Medical3 provides a unique opportunity to study this problem on a low-field system designed for point-of-care (POC) and emergency imaging. At this field strength, we can examine the effect of reducing the number of excitations (NEX) and undersampling at standard NEX to ultimately define a protocol that is “as fast as clinically useful”. Doing so could help make MRI the modality of choice for triaging neurological indications in emergency medicine, increase patient throughput, and reduce overall burden on hospital resources.
It was previously demonstrated that various objective image quality metrics (IQMs) can be correlated with radiologists’ expert opinions of image quality4. We now aim to apply these IQMs to retrospectively accelerated data to calibrate a relationship between IQMs and radiologist confidence in answering pointed clinical questions relevant to the example of triaging stroke patients.
Methods
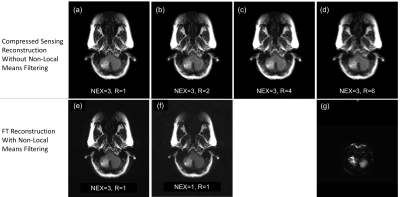
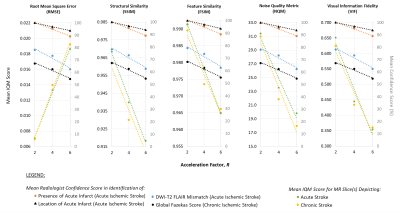
Data were acquired from eight patients (4F, 4M, average age 65y) admitted to hospital after an acute stroke. Following completion of their clinical care, patients were scanned on the 0.5T MRI system3 under a NSH REB-approved protocol. The protocol included an axial T2 FLAIR sequence (NEX=3, 250x216 matrix, scan time 266s) and an axial DWI sequence (2x parallel imaging, 120x120 matrix, scan time 97s, b=0 and 1000).FLAIR images were reconstructed with NEX=3 and NEX=1 using a standard FT pipeline, and filtered post-reconstruction via non-local (NL) means. FLAIR images (NEX = 3, unfiltered) were also degraded by retrospectively undersampling k-space (R=2,4,6), followed by compressed sensing (CS) reconstruction (𝓁1-wavelet sparsity, regularization factor 0.01) via the BART Toolbox5, without post-reconstruction filtering. RMSE, SSIM6, FSIM7, NQM8, and VIF9 were calculated for each degraded image. Each dataset consisted of a reference image and its corresponding degraded images, yielding 6 images per patient (Figures 1 and 2).
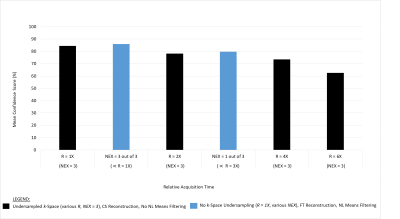
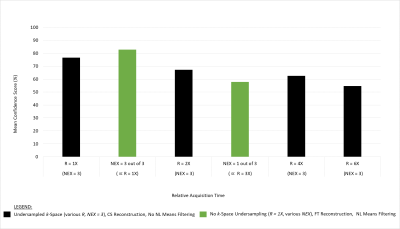
All FLAIR images, alongside corresponding DWI images and ADC maps, were shown to two board-certified radiologists who were asked a series of questions related to their ability to identify diagnostically relevant features of both acute and chronic ischemic stroke. They were also asked to rank their confidence in these identifications on a Likert scale (1-5, 1=0% confidence, 5=100% confidence). To date, our analysis has focused on identifying trends between scan time reduction, IQMs, and radiologist confidence, as well as determining the average confidence for a given relative acquisition time.
Results and Discussion
Figure 3 illustrates relationships between CS acceleration factor, image quality as measured by IQMs, and average radiologist confidence in identifying clinical features of stroke. These results demonstrate that IQMs may be a useful surrogate for radiologist confidence in identifying presence and location of ischemic stroke, in identifying a DWI-T2FLAIR mismatch, and in assigning a global Fazekas score for chronic stroke.Furthermore, we have shown that a decrease in projected acquisition time from 266s to 44.3s reduces the average radiologist confidence, at most, by 23% and 28% for DWI-T2FLAIR mismatch identification and assignment of a global Fazekas score, respectively (Figure 4). This reduced acquisition time is clearly beneficial for acute stroke scenarios, but valuable information on chronic stroke can also be gained from these accelerated scans. There is, therefore, potential to investigate acute and chronic scans in tandem, further reducing the overall burden on hospital resources.
We have additionally demonstrated that the reconstruction method has an impact on radiologist confidence scores, since filtered NEX=3 (FT reconstruction) images yielded slightly higher average confidence scores than unfiltered NEX=3 images (CS reconstruction), despite being produced from the same percentage of k-space data.
It is important to note that the trends presented here are indicative of radiologist confidence for the specific questions asked; however, the method can be applied to other applications for which accelerated scans would be beneficial, and to other areas which are well depicted with low-field imaging, such as imaging of orbits or the internal auditory canal.
Conclusions and Future Work
This study demonstrates that acquisition time on a low-field, POC MRI system can be significantly reduced without impacting radiologists’ confidence in answering questions clinically relevant to triage in the context of acute and chronic stroke.While general trends have been observed, future work will include a larger data set, such that the statistical significance of these trends can be determined. Since radiologists' confidence scores across all acceleration factors and NEX values tested remained very high for all questions examined in this study, a wider range of acceleration will be explored, including increased undersampling at NEX=3 (R>6) and undersampling with variable density NEX. IQM values will be used to help determine which combinations of acceleration are appropriate for further radiologist assessment. We will also include more difficult patient populations, such as those with strokes that do not appear on initial CT scans.
Acknowledgements
Funding for this research was provided by grants from Research Nova Scotia, NSERC Discovery program, Brain Repair Centre Knowledge Translation program and by scholarships from NSERC CGS-M program, Exxon Mobil Canada Ltd. Post-Graduate Scholarship, and the A.S. Mowat Prize.References
1. Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuck AM, et al. Magnetic Resonance Imaging and Computed Tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet 2007;369(9558):293.
2. Provost C, Soudant M, Legrand L, Ben Hassen W, Xie Y, Soize S, et al. Magnetic resonance imaging or computed tomography before treatment in acute ischemic stroke: Effect on workflow and functional outcome. Stroke 2019;50(3):659–64.
3. Stainsby JA, Bindseil GA, Connell IRO, Thevathasan G, Curtis AT, Beatty PJ, Harris CT, Wiens CN, and Panther A. Imaging at 0.5 T with high-performance system components. Proc. ISMRM 2019, no.1194.
4. Mason A, Rioux J, Clarke SE, Costa A, Schmidt M, Keough V, Huynh T, Beyea SD. Comparison of Objective Image Quality Metrics to Expert Radiologists' Scoring of Diagnostic Quality of MR Images. IEEE Trans Med Imaging 2020 Apr;39(4):1064-1072.
5. BART Toolbox for Computational Magnetic Resonance Imaging, DOI: 10.5281/zenodo.592960
6. Wang Z, Bovik AC, Sheikh HR, Simoncelli EP. Image Quality Assessment: From Error Visibility to Structural Similarity. IEEE Trans. Image Process 2004;13(4):600–612.
7. Zhang L, Zhang L, Mou X, Zhang D. FSIM: A Feature Similarity Index for Image Quality Assessment. IEEE Trans. Image Process 2011;20(8):2378–2386.
8. Damera-Venkata N, Kite TD, Geisler WS, Evans BL, Bovik AC. Image quality assessment based on a degradation model. IEEE Trans. Image Process 2000;9(4):636–650.
9. Sheikh HR, Bovik AC. Image information and visual quality. IEEE Trans. Image Process 2006;15(2):430–444.
Figures