0628
Disposable Point-of-care Portable Perfusion Phantom for Accurate Quantitative DCE-MRI1University of Alabama at Birmingham, Birmingham, AL, United States, 2Objective Design, Birmingham, AL, United States, 3Vanderbilt University Medical Center, Nashville, TN, United States, 4University of Texas, Austin, TX, United States
Synopsis
A new point-of-care portable perfusion phantom was developed to reduce inter- and intra-scanner variability of quantitative dynamic contrast enhanced magnetic resonance imaging (DCE-MRI). This device is disposable, easily operable, and conveniently deliverable for widespread, routine clinical use. As this device has high repeatability (intraclass correlation coefficient = 0.997), it can be utilized to improve the accuracy of quantitative DCE-MRI based analysis of many diseases including cancer.
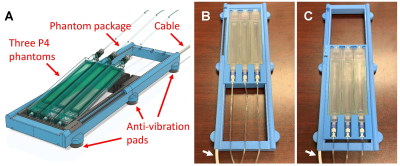
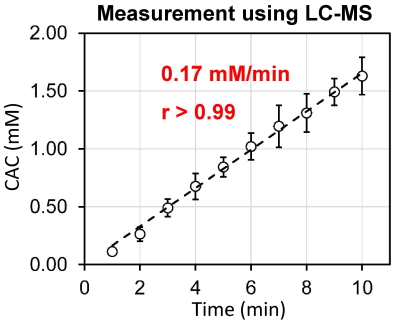
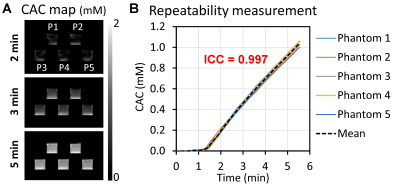
Methods: Our new disposable P4 phantom (see Fig. 1) is composed of top and bottom chambers with a semi-permeable membrane (pore size: 12~14 kDa) placed between them. The top chamber measures 1 × 15 × 150 mm (height × width × length), and the bottom chamber measures 15 × 15 × 150 mm. The top half has a ridge that protrudes along the perimeter of the top chamber, while the bottom half has a channel around it to accept the ridge. The membrane is placed such that the ridge and channel enclose it when the two halves are combined, clamping it into place and maintaining flatness. Both top and bottom chambers of the P4 phantom are filled with degassed/deionized water. To prevent water leakage that creates bubbles that cause variation in phantom performance, epoxy is used as a gasket between the two halves to prevent water leakage. The inlet and outlets of the phantom are closed with caps. Before use, the caps are removed, and a tube filled with an MR contrast agent is connected to the inlet. A computational fluid-dynamics (CFD) model was employed to optimize the top chamber geometry such that over 99% of the water would be displaced by the contrast agent infused into the top chamber. The CFD model was validated with samples collected from the top chamber using Liquid Chromatography–Mass Spectrometry (LC-MS). LC-MS also was utilized to measure the contrast enhancement curve (CEC) of the phantom. Two holes were drilled in the side of the bottom chamber and a 0.25 ml sample was extracted every minute for ten minutes after infusing 4 ml of gadoteridol (100 mM) at a constant rate (0.24 ml/s) into the top chamber. This process was repeated ten times for a total of 100 samples. The repeatability of the CEC was evaluated using DCE-MRI with five P4 phantoms located at the center of a single 3T MRI scanner (SIEMENS Prisma). A new phantom package (see Fig. 2) was designed to house up to three phantoms. The cassette was connected to a position-finder via a polymer and carbon-fiber cable system allowing an operator to adjust the cassette’s position by ±7.5 cm. A new patient bed (see Fig. 3) was made with wooden platforms (height × width × length = 6 × 48 × 206 cm, weight = 6 kg). The bed structure was configured using finite element analysis to support up to 136 kg of body weight when the subject sits on the bed. Using the cable controller indicated with an arrow at the end of the bed, the phantom’s location can be adjusted without interfering a human subject inside an MRI scanner.
Results: No bubble formation was observed in epoxy-sealed phantoms for at least four months. A CFD model of the top chamber geometry produced post-infusion gadoteridol purity of 99.2%, when 4 ml of gadoteridol is infused at a rate of 0.24 ml/s over 16.67 seconds. Figure 4 shows the CEC of the P4 phantom measured with LC-MS, confirming a linear increase (0.17 mM/min) of contrast-agent concentration in the phantom with 96% accuracy. Figure 5 shows the repeatability of the P4 phantom. Figure 5A shows the contrast agent concentration (CAC) maps of five phantoms (P1-P5) at 2, 3, and 5 minutes after the imaging initiation. Figure 5B shows the CECs of the phantoms. The intraclass correlation coefficient of the CECs was 0.997.
Discussion: We developed a new disposable P4 phantom and accompanying equipment for accurate quantitative DCE-MRI measurement in the routine clinical setting. The data consistency across different scanners and acquisition times will facilitate multi-institutional studies for drug development as well as improving diagnosis and prognosis accuracy of many diseases including cancer.
Acknowledgements
No acknowledgement found.References
1. Kim H., Mousa M., Schexnailder P., Hergenrother R., Bolding M., Ntsikoussalabongui B., Thomas V., Morgan, D. E., “Portable perfusion phantom for quantitative DCE‐MRI of the abdomen,” Medical Physics, 44: 5198-5209, 2017. 2.
2. Kim H., Thomas J. V., Nix J. W., Gordetsky J. B., Li Y., Rais-Bahrami S., “Portable Perfusion Phantom Offers Quantitative Dynamic Contrast-Enhanced Magnetic Resonance Imaging for Accurate Prostate Cancer Grade Stratification: A Pilot Study,” Academic Radiology, 2020 [Epub ahead of print].
Figures