0605
The feasibility of an optimized Faster R-CNN in detection and differentiation HT from PTMC Using high b-value DWI with RESOLVE1Collaborative Innovation Center, Institute of Software, Chinese Academy of Sciences, Beijing, China, 2University of Chinese Academy of Sciences, Beijing, China, 3Department of Radiology, PLA 6th medical center, Beijing, China, 4MR Scientific Marketing, Siemens Healthcare, Beijing, China, 5School of Computer Science and Technology, Beijing Institute of Technology, Beijing, China, 6State Key Laboratory of Computer Science, Institute of Software, Chinese Academy of Sciences, Beijing, China
Synopsis
In this study, we optimized a Faster R-CNN algorithm through constraining anchor boxes generated by Region Proposal Network (RPN) based on prior knowledge, and evaluated the feasibility of the optimized model in detecting and differentiating Hashimoto's thyroiditis (HT) from papillary thyroid microcarcinomas (PTMC) based on high b-value (2000 sec/mm2) diffusion-weighted images that acquired with readout segmentation of long variable echo-trains (RESOLVE) sequence. The study indicated that our model based on high b-value (2000 sec/mm2) DWI images demonstrated great potential as a new inspection tool in the diagnosis of benign and malignant thyroid micronodules.
Background and Purpose
Accurate diagnosis of benign or malignant thyroid micronodules (greatest diameter≤10 mm), especially Hashimoto's thyroiditis (HT) and papillary thyroid microcarcinomas (PTMC), is crucial in assessing micronodule risk and selecting optimal regimen1-3. However, it is a tough task for experienced sonographers and clinical specialists to make accurate judgments by using ultrasonography, considering the lack of clear diagnostic features1. Previous studies have confirmed that high b-value (2000 sec/mm2) DWI images may possess great value in the diagnosis of benign and malignant thyroid micronodules4. So, based on high b-value (2000 sec/mm2) DWI images, this study evaluate the feasibility of optimized deep learning algorithm in detecting and differentiating HT and PTMC.Materials and Methods
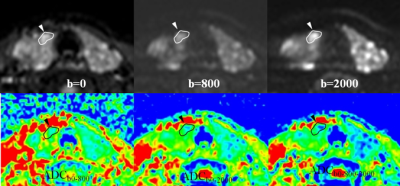
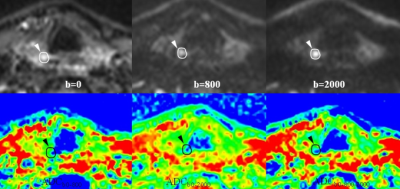
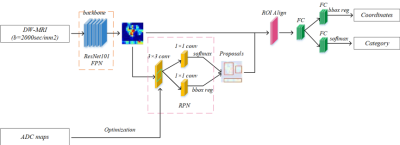
A total of 120 patients were randomly divided into two cohorts based on benign and malignant micronodules, i.e., the training cohort (80% of samples) and the testing cohort (20% of samples). The training cohort included 96 patients (nHT = 39 and nPTMC = 57), the testing cohort included 24 patients (nHT = 10 and nPTMC = 14). And no significant differences were found between the training cohort and testing cohort in terms of age, gender, micronodule location, and so on. All patients had undergone MRI examinations with a 3.0T scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) equipped with a dedicated 8-channel bilateral surface coil for the neck (Chenguang Medical Technologies CO., LTD, Shanghai, China) and a 4-channel soft surface coil for thoracic entrance (Siemens Healthcare Sector, Erlangen, Germany). The high b-value DWI images were obtained by using multi-shot readout segmentation of long variable echo-trains (RESOLVE) with the following sequence parameters: repetition time = 6200ms, echo time = 74/115ms, fat suppression is frequency-selective, flip angle = 180°, section thickness = 3mm, section interval = 0.3mm, field-of-view = 175mm×175mm, imaging matrix = 174×174, number of slices = 24, bandwidth = 685 Hz/pixel, parallel acquisition factor = 2, readout segments = 7, b = 0/800/2000 sec/mm2, average = 1/1/4, and the acquisition time is 14 min 11 sec. ADC maps were obtained by calculating ADC in each pixel of each slice with the three sets of DW-MRI based on different b-values (0, 800, 2000 sec/mm2): ADCb0-800, ADCb0-2000, ADCb0-800-2000. In order to explore the feasibility of high b-value DW-MRI with RESOLVE in automatically detecting micronodules and assessing micronodule risk, the computer-aided diagnosis (CAD) method was introduced. Considering its powerful representation learning ability, a Faster R-CNN algorithm was selected as the detection and classification model, which performs higher accuracy and lower error rate. The backbone of network was ResNet-101 and was initialized from ImageNet. In addition, we set 3 optimized sizes ($$$scales=[4,8,16]$$$) and 3 optimized aspect ratios ($$$ratios=[0.5,1,2]$$$) for constraining anchor boxes of RPN based on prior knowledge that the greatest diameter of micronodules is less than or equal to 10mm, and their aspect ratios (height divided by width) roughly range from 0.5 to 2.0. The learning rate of network was first set to 0.00003 for 30k iterations, then was set to 0.0003 for another 30k iterations in the training phase. The performance of model was evaluated by the examples of detection results and the average precision (AP).Results
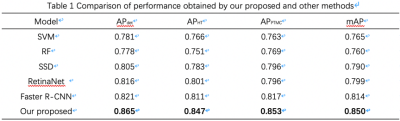
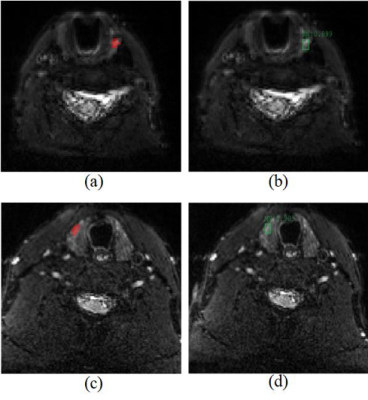
In this experiment, we have found that Faster R-CNN with clinical prior knowledge can achieve the detection and classification between HT and PTMC automatically, and get the highest accuracy compared with other methods (Table 1). The AP of detection in HT and PTMC, HT, PTMC, and average is 0.865, 0.847, 0.853 and 0.850, respectively. Some typical detection examples shown in Figure 4 as qualitatively comparison results.Discussions
It is important to diagnose the benign and malignant of micronodules accurately for evaluating risk. However, in clinical diagnosis, it is difficult to make judgments by using sonographic characteristics, considering the tiny lesion of thyroid micronodules, i.e., HT and PTMC. DW-MRI can provide information about tumor pathological and functional features such as cellular density and proliferation activity. Previous studies have confirmed that high b-value DWI images may possess great potential in the diagnosis of benign and malignant thyroid micronodules, especially on images acquired by using multi-shot readout segmentation of long variable echo-trains (RESOLVE) which can improve image quality of the small and complex anatomic structure with less susceptibility artifacts, blurring from T2 signal decay and distortion5. To reduce the omission and misdiagnosis rate, an advanced deep learning method, i.e., Faster R-CNN, is used to detect and distinguish HT and PTMC, which is initialized from ImageNet for preventing network overfitting. The anchor box of RPN is optimized by the morphological size of micronodules to generate better objective location. Through evaluation, a positive result was gained which may raise the diagnosing accuracy in future.Conclusions
The study indicated that based on high b-value (2000 sec/mm2) DWI images, our optimized Faster R-CNN model demonstrated great potential as a new inspection tool to for the diagnosis of benign and malignant thyroid micronodules.Acknowledgements
This research was funded by National Key R&D Program of China from Ministry of Science and Technology (2017YFB1002303).References
1. Haugen B R, Alexander E K, Bible K C, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1-133.
2. Cho B Y, Choi H S, Park Y J, et al. Changes in the clinicopathological characteristics and outcomes of thyroid cancer in Korea over the past four decades. Thyroid. 2013;23(7):797-804.
3. Londero S C, Krogdahl A, Bastholt L, et al. Papillary thyroid carcinoma in Denmark, 1996–2008: outcome and evaluation of established prognostic scoring systems in a prospective national cohort. Thyroid. 2015;25(1):78-84.
4. Schob S, Voigt P, Bure L, et al. Diffusion-weighted imaging using a readout-segmented, multishot EPI sequence at 3 T distinguishes between morphologically differentiated and undifferentiated subtypes of thyroid carcinoma—a preliminary study. Translational oncology. 2016;9(5):403-410.
5. Wang Q, Guo Y, Zhang J, et al. Diagnostic value of high b-value (2000 s/mm2) DWI for thyroid micronodules. Medicine. 2019;98(10):e14298.
Figures