0593
Registration on different lung volumes and its influence on ventilation and perfusion parameters derived by phase-resolved functional lung MRI1Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Centre for Lung Research (DZL), Hannover, Germany
Synopsis
Correction of lung motion is a mandatory step for the voxel-wise signal analysis of Fourier Decomposion (FD) based methods, such as phase-resolved functional lung (PREFUL) MRI. Usually, all images are registered towards one fixed image in intermediate lung position. In this work, a group oriented registration approach with three different target images (expiration, middle, inspiration) was tested and the influence on functional parameters derived by PREFUL was evaluated in 41 study participants. While small significant differences were observed, high absolute agreement of all functional ventilation and perfusion parameters was found indenpedent on the chosen target volume.
Introduction
Non-contrast-enhanced ventilation (V) and perfusion (Q) assessment of human lungs gained interest in the last years. Phase-resolved functional lung (PREFUL)1 imaging, offers sensitive measurement of regional V and Q dynamics2. The correction for the lung and vasculature motion is necessary for the voxel-wise analysis of signal time-series in free breathing MR acquisitions. Conventionally, an image in the intermediate lung position is chosen as the target image for the registration. But using the group-oriented registration3 with small step-by-step registrations, large deformations (peak-inspiration to peak-expiration or vice versa) are feasible. Since the lung inflation affects the pulmonary anatomy, a change in the functional parameters is expected4–6. Until now the influence of different respiration state target images on the functional V and Q PREFUL parameters was not assessed. Therefore, the purpose of this work was to vary the target image used for registration and evaluate its influence on V and Q parameters.Methods
Twelve healthy volunteers (6 females, median age: 29.5 years) and twenty-nine patients with pulmonary diseases (14 females, median age: 52 years) underwent imaging on a 1.5T MR-scanner. Images of three coronal slices were acquired using a spoiled gradient echo sequence with the following parameters: TE 0.67/0.82 ms, TR 3 ms, flip angle 5°/8°, FOV 50 x 50 cm2/45 x 45 cm2, slice thickness 15 mm, matrix size 128x128 interpolated to 256x256, pixel bandwidth 1500/1502 Hz/pixel, total TA 58 seconds for 200 images per slice.Group-oriented registration3 towards expiration/middle respiratory state/inspiration was performed using Advanced Normalization Tools (ANTs)7. The PREFUL postprocessing described previously1 was executed to derive V and Q parameters.
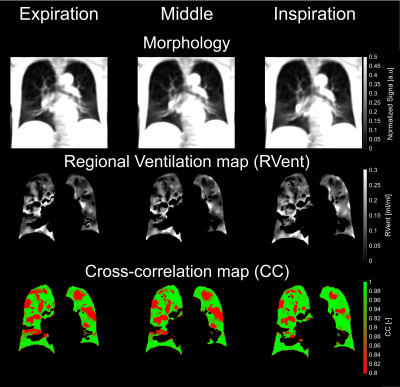
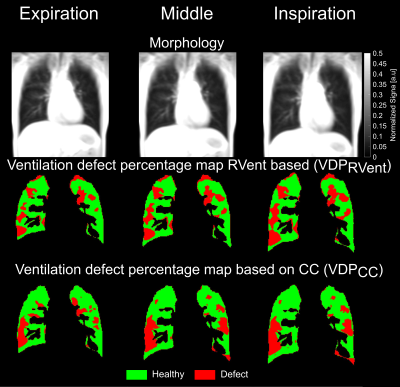
For V, regional ventilation (RVent) maps were computed8. The RVent dynamics was further analyzed using flow-volume loops (FVL)9. Similarity of all FVLs to a healthy-reference FVL10 was measured by the cross-correlation, which resulted in a cross-correlation (CC) map. Further, ventilation defect maps (VDPRVent and VDPCC) were generated using published thresholds10,11.
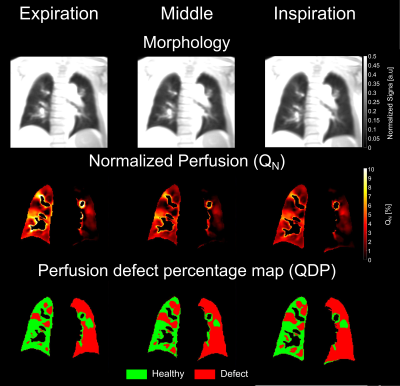
For Q, a perfusion-weighted image was chosen according to Behrendt et al.12 and normalized to the signal of full-blood-voxels (QN). Also, perfusion defect maps based on QN (QDP) were constructed with the fixed threshold of 2%.
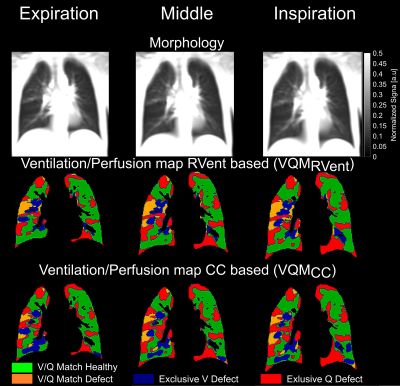
Since V and Q are spatially aligned, V/Q maps were generated for both combinations (VDPRVent/QDP and VDPCC/QDP) and V/Q match was computed for healthy (VQMHealthyRVent and VQMHealthyCC) and defect areas (VQMDefectRVent and VQMDefectCC).
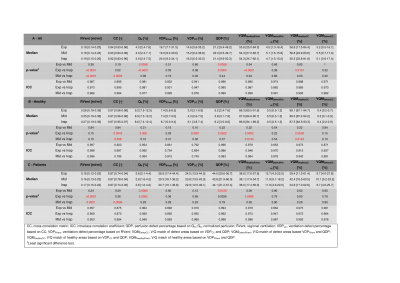
Differences between V and Q parameters (median RVent, median CC, median QN, total VDPRVent, total VDPCC, total QDP, total VQMHealthyRVent, total VQMHealthyCC, total VQMDefectRVent and total VQMDefectCC) derived with different target images were tested for significance using least significant difference test with alpha level of 0.0167 (Bonferroni corrected). A total agreement between pairs of V and Q parameters was assessed by intraclass correlation coefficients (ICC).
Results
Median and interquartile range of V and Q parameters, respective p-values and ICC coefficients are presented in Table 1. A good visual agreement of all PREFUL parameters, derived for different target images, is shown in Figure 1-4.When comparing all study participants, the most pronounced differences were found between registration towards inspiration and expiration, where five parameters were significantly different (RVent, QN, QDP, VQMHealthyRVent, VQMHealtyCC - all p<0.015).
In healthy volunteers, the lowest median defect percentage values (VDPRVent, VDPCC and QDP) were found, when registering to expiration images and the highest median defect percentage values for registration towards inspiration images. Six parameters (CC, QN, VDPCC, QDP, VQMHealthyRVent, VQMHealthyCC) were found to be statistically different in the comparison between registration to expiration and inspiration (all p<0.008).
In patients only, three parameters (RVent, QN and VQMHealthyRVent) were significantly different in the comparison between registration towards expiration and inspiration (all p<0.01).
Good to excellent absolute agreement was found in all comparisons (ICC range: 0.697-0.999). Lower ICC values were seen for VDPRVent, VDPCC and CC parameter.
Discussion
This study demonstrates the influence of the chosen target image for the registration on 2D-PREFUL derived V and Q parameters. Although, some of the comparisons showed significant differences between derived parameters, the absolute agreement of all parameters was very high.As expected, the majority of differences was mostly pronounced in the comparison between registration towards expiration and inspiration. It has been shown, that perfusion values derived by dynamic-contrast-enhanced (DCE) imaging are dependent on the breathold state5. This supports slightly higher perfusion values observed in our study when registering towards expiration.
The RVent parameter, as an absolute ventilation marker was not significantly changed with the different target volume in healthy volunteers, indicating for variability due to registration itself. Furthermore, the ICC values were decreased for defect percentage values (VDPRVent and VDPCC) suggesting for additional uncertainities caused by thresholds.
Also, in healthy volunteers, the less V and Q defects were seen for registration towards expiration. Since the expiration state takes longer during normal tidal breathing than inspiration, the image sharpness of expiratory images is increased. Thus, the registration procedure might be more accurate when registering towards expiration.
Considering through-plane motion, results for more far anterior and posterior slices might differ. However most current studies go without full lung acquisition using a similar slice acquisition strategy as described in this study.
Conclusion
Different target volumes for registration showed significantly different but small variations in the final PREFUL parameters.Acknowledgements
No acknowledgement found.References
1. Voskrebenzev A, Gutberlet M, Klimeš F, et al. Feasibility of quantitative regional ventilation and perfusion mapping with phase-resolved functional lung (PREFUL) MRI in healthy volunteers and COPD, CTEPH, and CF patients. Magn Reson Med. 2018;79(4):2306-2314. doi:10.1002/mrm.26893
2. Vogel-Claussen J, Schönfeld CO, Kaireit TF, et al. Effect of indacaterol/glycopyrronium on pulmonary perfusion and ventilation in hyperinflated patients with chronic obstructive pulmonary disease (CLAIM) a double-blind, randomized, crossover trial. Am J Respir Crit Care Med. 2019;199(9):1086-1096. doi:10.1164/rccm.201805-0995OC
3. Voskrebenzev A, Gutberlet M, Kaireit TF, Wacker F, Vogel-Claussen J. Low-pass imaging of dynamic acquisitions (LIDA) with a group-oriented registration (GOREG) for proton MR imaging of lung ventilation. Magn Reson Med. 2017;78(4):1496-1505. doi:10.1002/mrm.26526
4. Mai VM, Chen Q, Bankier AA, et al. Effect of lung inflation on arterial spin labeling signal in MR perfusion imaging of human lung. J Magn Reson Imaging. 2001;13(6):954-959. doi:10.1002/jmri.1137
5. Fink C, Ley S, Risse F, et al. Effect of Inspiratory and Expiratory Breathhold on Pulmonary Perfusion. Invest Radiol. 2005;40(2):72-79. doi:10.1097/01.rli.0000149252.42679.78
6. Hughes PJC, Smith L, Chan HF, et al. Assessment of the influence of lung inflation state on the quantitative parameters derived from hyperpolarized gas lung ventilation MRI in healthy volunteers. J Appl Physiol. 2019;126(1):183-192. doi:10.1152/japplphysiol.00464.2018
7. Avants BB, Tustison NJ, Song G, Cook PA, Klein A, Gee JC. A reproducible evaluation of ANTs similarity metric performance in brain image registration. Neuroimage. 2011;54(3):2033-2044. doi:10.1016/j.neuroimage.2010.09.025
8. Klimeš F, Voskrebenzev A, Gutberlet M, et al. Free‐breathing quantification of regional ventilation derived by phase‐resolved functional lung (PREFUL) MRI. NMR Biomed. 2019;(February):e4088. doi:10.1002/nbm.4088
9. Voskrebenzev A, Klimeš F, Gutberlet M, et al. Imaging-Based Spirometry in Chronic Obstructive Pulmonary Disease (COPD) Patients using Phase Resolved Functional Lung Imaging (PREFUL). Proc Intl Soc Mag Reson Med 26. 2018:1079. http://indexsmart.mirasmart.com/ISMRM2018/PDFfiles/1079.html.
10. Moher Alsady T, Voskrebenzev A, Greer M, et al. MRI‐derived regional flow‐volume loop parameters detect early‐stage chronic lung allograft dysfunction. J Magn Reson Imaging. 2019;L:1-10. doi:10.1002/jmri.26799
11. Kaireit TF, Kern A, Voskrebenzev A, et al. Flow Volume Loop and Regional Ventilation Assessment Using Phase‐Resolved Functional Lung (PREFUL) MRI: Comparison With 129Xenon Ventilation MRI and Lung Function Testing. J Magn Reson Imaging. 2020;L:jmri.27452. doi:10.1002/jmri.27452
12. Behrendt L, Voskrebenzev A, Klimeš F, et al. Validation of Automated Perfusion‐Weighted Phase‐Resolved Functional Lung (PREFUL)‐MRI in Patients With Pulmonary Diseases. J Magn Reson Imaging. December 2019:jmri.27027. doi:10.1002/jmri.27027
Figures