0482
Hilar cholangiocarcinoma evaluation using zoomed echo-planar DW imaging with 2D spatial-selective radiofrequency excitation pulses1Department of MR Imaging, the First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 2MR Collaboration, Siemens Healthcare Ltd, Beijing, China
Synopsis
We investigated the feasibility of using and the resultant image quality of zoomed diffusion-weighted echo-planar imaging (z-EPI) for hilar cholangiocarcinoma assessments. Compared with conventional single-shot EPI (c-EPI), z-EPI showed better delineation of anatomic structures in the hepatic hilar region, better lesion conspicuity, and overall higher image quality. Bile duct wall lesion delineations and lumens were also improved in z-EPI in four of 16 patients. These findings suggest that z-EPI may be preferred for improved imaging of hilar cholangiocarcinoma.
Abstract
PurposeDWI images obtained with conventional single-shot echo-planar imaging (EPI) are often degraded by lower spatial resolution, susceptibility artifacts, and image blurring [1-3]. As opposed to conventional EPI (c-EPI) DWI, zoomed EPI DWI (z-EPI) utilizes two-dimensional spatial-selective radiofrequency excitation pulses combined with reduced field of view (FOV) in the phase-encoding direction (‘zoomed’). This could lead to superior image quality with reduced spatial distortions and artifacts and improved identification of small anatomic structures [4, 5]. Published works using this method have mainly concentrated on the pancreas, kidney, prostate, spinal cord, and head and neck regions [4-12]; however, no literature regarding the use of z-EPI to examine the hepatic hilar region exists. Therefore, we aimed to investigate the feasibility of using and resultant image quality of z-EPI in hilar cholangiocarcinoma compared with c-EPI.
Method
Both c-EPI and z-EPI (b values = 50 and 800 s/mm2) were performed on a 3T MR system (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) in 16 patients with histopathologically confirmed hilar cholangiocarcinoma. The acquisition parameters of c-EPI DWI were: TR/TE = 4500/56 ms; FOV = 350×292 mm2; matrix = 158×121; slice thickness = 5 mm; reconstructed voxel size 2.2×2.2×5.0 mm3; parallel acceleration factor = 2; acquisition time = 1 min 52 sec. The parameters of z-EPI DWI were: TR/TE = 2000/61 ms; FOV = 230×120 mm2; matrix = 154×50; slice thickness = 5 mm; reconstructed voxel size 1.5×1.5×5.0 mm3; parallel acceleration factor = 2; acquisition time = 1 min 53 sec. Two blinded radiologists performed independent retrospective quantitative assessments of the two imaging groups. Anatomic structural visualization, lesion conspicuity, artifact presence, and overall image quality were evaluated with a 4-point scale (anatomic structure visualization (1, poorly visualized anatomy and non-diagnostic; 2, fairly delineated hepatic hilus zone with margin blurring; 3, good delineation of hepatic hilus zones with sharp margins; 4, excellent sharpness of hepatic hilus zone), 2) lesion conspicuity (1, lesion not detectable; 2, simply lesion-to-background contrast recognized; 3, intermediate lesion-to-background contrast or high contrast with indistinct lesion margins seen; 4, excellent lesion-to background contrast and clear lesion margins), 3) artifacts (1, severe and non-diagnostic; 2, moderate; 3, mild; 4, absent) and 4) overall image quality as a sum of the above mentioned 3 parameters) and compared between the two sets of images. The ratio of hilar cholangiocarcinoma lesion size differences was measured on T2-weighted imaging and DWI images acquired from both EPI techniques. Statistical analyses were performed using the Student’s t-test and Wilcoxon signed-rank test, and differences were considered significant at the 5% level (p < 0.05).
Result
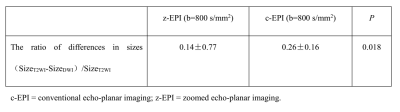
The hepatic hilar region was better delineated by visualization of anatomic structures, lesion conspicuity, and overall image quality using z-EPI compared with c-EPI (all p<0.05) (Table 1). Better lesion delineation of bile duct walls and lumens was seen in four patients with z-EPI compared with c-EPI (Figure 1). No significant differences were found between the two sequences for artifacts (p=0.876). The ratio of differences regarding hilar cholangiocarcinoma lesion sizes calculated from z-EPI was significantly lower than those calculated from c-EPI (p= 0.018, table 2).
Discussion
Abdominal DWI can be technically challenging due to distortion artifacts in the phase-encoding direction. z-EPI DWI has potentially better advantages over conventional single-shot EPI for using two-dimensional spatial-selective radiofrequency pulses to obtain reduced volumes while also achieving higher resolution and reducing distortions without unfolding artifacts [5, 13]. In addition, the hepatic hilar region DWI is less influenced by adjacent air and motion from the stomach and intestines. This is the first MRI study to evaluate the use and clinical application of z-EPI DWI to study the hepatic hilar region. The results indicate that z-EPI outperforms c-EPI in this region for anatomic structural visualization, lesion conspicuity, and overall image quality.
Conclusions
Compared with c-EPI DWI, z-EPI DWI showed remarkable improvements in overall image quality for the assessment of hilar cholangiocarcinoma lesions, including superiority in detecting and delineating lesions. These benefits could help radiologists to evaluate hilar cholangiocarcinoma lesions in greater detail. Further studies are warranted to determine if z-EPI could replace c-EPI in clinical settings.
Acknowledgements
No acknowledgement found.References
1. Bittencourt LK, Matos C, Coutinho AC Jr. Diffusion-weighted magnetic resonance imaging in the upper abdomen: technical issues and clinical applications. Magn Reson Imaging Clin N Am. 2011;19(1):111-131.
2. Dietrich O, Biffar A, Baur-Melnyk A, Reiser MF. Technical aspects of MR diffusion imaging of the body. Eur J Radiol. 2010;76(3):314-322.
3. Attenberger UI, Morelli J, Budjan J, et al. Fifty Years of Technological Innovation: Potential and Limitations of Current Technologies in Abdominal Magnetic Resonance Imaging and Computed Tomography. Invest Radiol. 2015;50(9):584-593.
4. Riffel P, Michaely HJ, Morelli JN, et al. Zoomed EPI-DWI of the pancreas using two-dimensional spatially-selective radiofrequency excitation pulses. PLoS One. 2014;9(3):e89468.
5. Thierfelder KM, Sommer WH, Dietrich O, et al. Parallel-transmit-accelerated spatially-selective excitation MRI for reduced-FOV diffusion-weighted-imaging of the pancreas. Eur J Radiol. 2014;83(10):1709-1714.
6. Thierfelder KM, Scherr MK, Notohamiprodjo M, et al. Diffusion-weighted MRI of the prostate: advantages of Zoomed EPI with parallel-transmit-accelerated 2D-selective excitation imaging. Eur Radiol. 2014;24(12):3233-3241.
7. Korn N, Kurhanewicz J, Banerjee S, Starobinets O, Saritas E, Noworolski S. Reduced-FOV excitation decreases susceptibility artifact in diffusion-weighted MRI with endorectal coil for prostate cancer detection. Magn Reson Imaging. 2015;33(1):56-62.
8. Rosenkrantz AB, Chandarana H, Pfeuffer J, et al. Zoomed echo-planar imaging using parallel transmission: impact on image quality of diffusion-weighted imaging of the prostate at 3T. Abdom Imaging. 2015;40(1):120-126.
9. Attenberger UI, Rathmann N, Sertdemir M, et al. Small Field-of-view single-shot EPI-DWI of the prostate: Evaluation of spatially-tailored two-dimensional radiofrequency excitation pulses. Z Med Phys. 2016;26(2):168-176.
10. He YL, Hausmann D, Morelli JN, Attenberger UI, Schoenberg SO, Riffel P. Renal zoomed EPI-DWI with spatially-selective radiofrequency excitation pulses in two dimensions. Eur J Radiol. 2016;85(10):1773-1777.
11. Seeger A, Klose U, Bischof F, Strobel J, Ernemann U, Hauser TK. Zoomed EPI DWI of Acute Spinal Ischemia Using a Parallel Transmission System. Clin Neuroradiol. 2016;26(2):177-182.
12. Riffel P, Michaely HJ, Morelli JN, et al. Zoomed EPI-DWI of the head and neck with two-dimensional, spatially-selective radiofrequency excitation pulses. Eur Radiol. 2014;24(10):2507-2512.
13. Rieseberg S, Frahm J, Finsterbusch J. Two-dimensional spatially-selective RF excitation pulses in echo-planar imaging. Magn Reson Med. 2002;47(6):1186-1193.
Figures
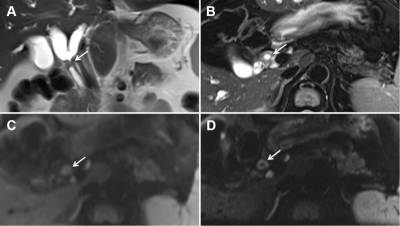
Figure 1. A 52-year-old man with hilar cholangiocarcinoma.
Coronal (A) and axial (B) T2-weighted magnetic resonance imaging images showing the hepatic duct (arrows) with wall thickening and mild hyperintensities. On conventional echo-planar (c-EPI) diffusion-weighted imaging (DWI) (C) and zoomed echo-planar imaging (z-EPI) DWI (D) obtained at b = 800 s/mm2, the common hepatic duct lesion is hyperintense. The thickened common hepatic duct wall is better delineated with z-EPI (arrow in D) than with c-EPI.