0479
Breath-hold 3D gradient- and spin-echo (GRASE) MRCP compared to compressed-sensing highly accelerated respiratory-triggered technique.1Radiology, Gifu University, Gifu, Japan, 2Radiology Services, Gifu University Hospital, Gifu, Japan
Synopsis
MR cholangiopancreatography (MRCP) plays an essential role in the noninvasive assessment of the biliary and pancreatic duct systems. Although the conventional respiratory-triggered three-dimensional turbo spin-echo (RT-3D-TSE) MRCP sequence has an excellent duct-to-periductal tissue contrast, the long acquisition time, over 5 minutes, has been a clinical burden. We assessed two types of ultrafast MRCP within 30 seconds of scan time. Breath-hold 3D gradient- and spin-echo (GRASE) MRCP provided better image quality and a reduced number of poor or non-diagnostic images compared to RT-3D-TSE MRCP highly accelerated with optimized integrated combination with parallel imaging and compressed-sensing technique (Compressed SENSE).
Introduction
MR cholangiopancreatography (MRCP) is widely used as a noninvasive modality for the anatomical evaluation of the pancreaticobiliary systems. The most common sequence used in three-dimensional (3D) MRCP is a respiratory-triggered 3D turbo spin-echo (RT-3D-TSE) sequence1. Although RT-3D-TSE MRCP can considerably contribute to a wide coverage, a thinner effective slice thickness, and high signal-to-noise ratio (SNR), the long acquisition time has been a clinical burden. Despite the combination of a faster gradient and a parallel imaging (PI) technique, for instance SENSE (sensitivity encoding), the acquisition time of RT-3D-TSE MRCP often exceeds 5 minutes, one of the longest sequences in abdominal MR imaging. Thus, there are unmet clinical needs to reduce the scan time for RT-3D-TSE MRCP.The recent development of the compressed-sensing (CS) technique, such as optimized integrated combination with SENSE PI and CS technique (Compressed-SENSE), has provided an option to achieve ultrafast 3D MRCP, with promising results demonstrated in some prior studies2,3. Although the method is promising, it is not enabled to be accelerated unlimitedly in routine clinical practice. On the other hand, a few approaches have been proposed to shorten the scan time and achieve 3D acquisition within a single breath-hold (BH), including the BH 3D gradient- and spin-echo (BH-3D-GRASE) technique4-6, 3D balanced steady-state free-precession (b-SSFP)7, or fast recovery fast spin-echo (FRFSE)8 sequences. Progress in the past a few years in MR hardware, including a more homogeneous B0 field and a more powerful gradient system with enhanced fidelity, has increased the potential of BH-3D-GRASE MRCP protocol for more clinical use.
To the best of our knowledge, there is no study to compare BH 3D MRCP to RT 3D MRCP with fast acquisition. Thus, we assessed two types of ultrafast MRCP within 30 seconds of acquisition time. We hypothesized that BH-3D-GRASE MRCP may contribute the better image quality compared to RT-3D-TSE MRCP highly accelerated with the Compressed-SENSE. The purpose of this study was to evaluate BH-3D-GRASE MRCP sequence compared to RT-3D-TSE MRCP highly accelerated with the Compressed-SENSE.
Materials and Methods
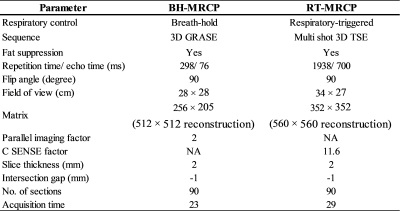
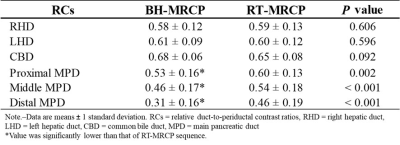
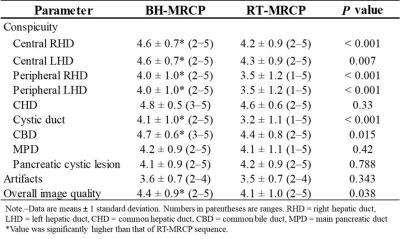
Institutional review board approval was obtained for this prospective HIPAA-compliant study. Fifty-eight consecutive patients (30 men, 28 women, age range 17‒86 years, mean age 67.2 years) with suspicious having pancreaticobiliary diseases underwent MRCP on a 3-T clinical scanner (Ingenia CX; Philips Healthcare, Best, The Netherlands) with a 32-channel phased-array receiver coil. All patients underwent BH-3D-GRASE MRCP with SENSE (BH-MRCP; SENSE factor, 2) and RT-3D-TSE MRCP highly accelerated with the Compressed-SENSE (RT-MRCP; C-SENSE factor, 11.6) in a random order. Scan parameters were demonstrated in Table 1. For quantitative image analyses, signal intensity (SI) of right hepatic duct (RHD), left hepatic duct (LHD), common bile duct (CBD), proximal, middle, and distal segments of main pancreatic duct (MPD), peribiliary ductal tissue, and peripancreatic ductal tissue were measured. The relative duct-to-periductal contrast ratios (RCs) of each pancreaticobiliary segments were calculated as (SIduct - SIperiduct)/ (SIduct + SIperiduct), respectively. For qualitative image analyses, two radiologists coincidentally graded conspicuity of central and peripheral segment of RHD and LHD, common hepatic duct (CHD), cystic duct, CBD, MPD and pancreatic cystic lesion, and overall image quality between the two sequences using a five-point rating scale (1 = non-diagnostic, 2 = poor, 3 = fair, 4 = good, and 5 = excellent). The degree of artifacts between the two sequences were also graded using a four-point rating scale (1 = severe, 2 = intermediate, 3 = minimal, and 4 = none). Quantitative measurements and qualitative scales between the two sequences were compared using paired t-test and Wilcoxson signed rank test, respectively. The number of scans with the poor or non-diagnostic image quality (score ≤ 2) in overall image quality between the two sequences was compared using Fisher’s exact test.Results
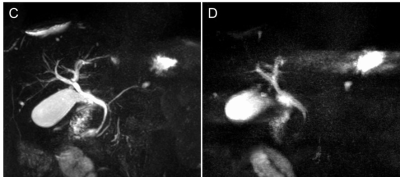
Mean acquisition time in BH-MRCP and RT-MRCP sequence was 23 and 29 seconds, respectively. Quantitative results were demonstrated in Table 2. RCs of all three segments of MPD in BH-MRCP were slightly lower than those in RT-MRCP (P ≤ 0.002). Qualitative results were demonstrated in Table 3. Conspicuity of central and peripheral segments of RHD and LHD, cystic duct, and CBD in BH-MRCP were significantly higher than those in RT-MRCP (P ≤ 0.015). Conspicuity of MPD and pancreatic cystic lesion was comparable between the two sequences. Overall image quality in BH-MRCP was significantly higher than that in RT-MRCP (P = 0.038, Fig. 1). In BH-MRCP, the number of scans with the poor or non-diagnostic image quality (score ≤ 2) in overall image quality was decreased compared with that in RT-MRCP [3.4% (2/58) vs. 8.6% (5/58), P = 0.242, Fig. 2].Discussion
Our results demonstrated that BH-MRCP achieved the better image quality compared to RT-MRCP within 30 seconds of acquisition time. RCs of in BH-MRCP were kept within the acceptable range compared to those in RT-MRCP. Respiratory-triggered technique was delicate method for patients with a shallow or irregular breathing rhythm4, as a result, conspicuity of biliary tracts in BH-MRCP were significantly superior to those in RT-MRCP. We believe that, in ultrafast MRCP sequence, BH-MRCP can contribute to improve the throughput time and could be valuable in clinical use.Conclusion
BH-MRCP provided better image quality and a reduced number of poor or non-diagnostic images compared to RT-MRCP.Acknowledgements
The authors of this abstract declare no relationships with any companies whose products or services may be related to the subject matter of the article.References
1. Lee JH, Lee SS, Kim JY, et al. Parallel imaging improves the image quality and duct visibility of breathhold two-dimensional thick-slab MR cholangiopancreatography. Journal of magnetic resonance imaging : JMRI 2014;39:269-75.
2. Nagata S, Goshima S, Noda Y, et al. Magnetic resonance cholangiopancreatography using optimized integrated combination with parallel imaging and compressed sensing technique. Abdominal radiology 2019;44:1766-72.
3. Tokoro H, Yamada A, Suzuki T, et al. Usefulness of breath-hold compressed sensing accelerated three-dimensional magnetic resonance cholangiopancreatography (MRCP) added to respiratory-gating conventional MRCP. European journal of radiology 2020;122:108765.
4. Nam JG, Lee JM, Kang HJ, et al. GRASE Revisited: breath-hold three-dimensional (3D) magnetic resonance cholangiopancreatography using a Gradient and Spin Echo (GRASE) technique at 3T. European radiology 2018;28:3721-8.
5. He M, Xu J, Sun Z, et al. Comparison and evaluation of the efficacy of compressed SENSE (CS) and gradient- and spin-echo (GRASE) in breath-hold (BH) magnetic resonance cholangiopancreatography (MRCP). Journal of magnetic resonance imaging : JMRI 2020;51:824-32.
6. Yoshida M, Nakaura T, Inoue T, et al. Magnetic resonance cholangiopancreatography with GRASE sequence at 3.0T: does it improve image quality and acquisition time as compared with 3D TSE? European radiology 2018;28:2436-43.
7. Glockner JF, Saranathan M, Bayram E, Lee CU. Breath-held MR cholangiopancreatography (MRCP) using a 3D Dixon fat-water separated balanced steady state free precession sequence. Magnetic resonance imaging 2013;31:1263-70.
8. Sodickson A, Mortele KJ, Barish MA, Zou KH, Thibodeau S, Tempany CM. Three-dimensional fast-recovery fast spin-echo MRCP: comparison with two-dimensional single-shot fast spin-echo techniques. Radiology 2006;238:549-59.
Figures