0376
Prognostic significance of MRI-detected mesorectal fat thickness in rectal cancer; a risk factor for distance metastasis1Department of Radiology, Tongji Hospital, Tongji Medical College of Huazhong University of Science and Technology, Wuhan, China
Synopsis
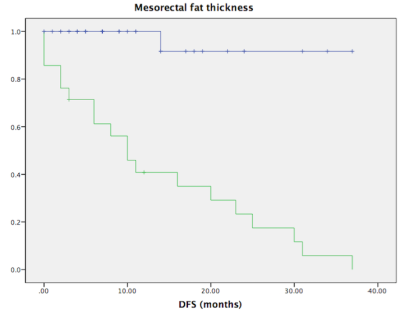
Our study got a step closer to probable cause of the poor prognosis in rectal cancer in obese patients. The correlation of the area within mesorectum with BMI and also the correlation between the mesorectal fat thickness and distant metastasis signifies the need of selection of optimum treatment modality for obese patients in rectal cancer. This preliminary study may shed some light on the current scenario and show probable direction for the solution. Selection of different treatment modalities and new surgical techniques may be required to improve the prognosis.
Introduction
Clinicopathological and environmental factors such as extramural vascular invasion, lymph-node invasion, perineural invasion, depth of tumor invasion, carcinoembryonic antigen (CEA), overweight and obesity are considered as independent risk factors for colorectal cancers. Furthermore, obesity is related to poor prognosis, surgical difficulty and worst surgical outcomes in rectal cancer. Therefore, we primarily aimed to investigate relationship between MRI detected mesorectal fat and BMI. Furthermore, investigate the impact of MRI detected mesorectal fat distant metastasis in patients with rectal cancer.Methods
Post-operative histopathologically confirmed T3 rectal cancer patients without previous treatment from July 2016 to December 2019 were enrolled for this study. Two blinded radiologists evaluated MRI detected extramural vascular invasion (mrEMVI) status, MRI detected depth of tumor extension, MRI-detected mesorectal fat thickness, area within mesorectum, mesorectum thickness and fat buffer thickness. The results along with other clinical characteristics (age, sex, tumor location, tumor direction, lymphatic invasion, perineural invasion, mrEMVI, tumor differentiation, BMI, types of surgery, CEA, CA724 and CA199) were then correlated with distant metastases to determine the risk factors using univariate and multivariate analysis. Cox regression analysis was used to estimate independent risk factors for disease-free survival (DFS).Results
In 77 patients (58.9±11.69 years), 33 patients were confirmed to be mrEMVI-positive. The mesorectal thickness, area within mesorectum, area inside rectum, fat buffer area and BMI were 4.79 ± 2.86 mm, 2708 ± 513.29 mm2, 951.88 ± 288.42 mm2, 1756.42 ± 448.56 mm2 and 22.43 ± 3.70 kg/m2 respectively. Area within mesorectum (p=0.02), area inside rectum (p=0.05) and fat buffer area (p=0.02) showed significant correlation with BMI. Univariate analysis revealed six factors significantly associated with distant metastasis: mrEMVI (p<0.00; odd ratio=0.03), MRI detected depth of tumor extension (p=0.01; odd ratio=2.0), tumor location (p<0.00; odd ratio=0.002), MRI detected mesorectal fat thickness (p<0.00; odd ratio=4.96), area within mesorectum (p=0.001; odd ratio=3.54), and fat buffer thickness (p<0.00; odd ratio=4.97). Multivariate analysis revealed only MRI-detected mesorectal fat thickness to be significantly associated with distant metastasis. 3-year disease-free survival rates were 97.2% and 9.5% (P <0.001) in patients with mesorectal fat thickness >3.325mm and <3.325mm groups.Conclusion
Area within mesorectum, area inside rectum and fat buffer area has significant correlation with BMI. MRI-detected mesorectal fat thickness is an independent risk factor for distant metastasis in rectal cancer.Acknowledgements
Dr. Tripathi Pratik developed the original idea and the protocol, abstracted and analysed data. Dr. Zhen Li, Dr. Yaqi Shen, Dr. Xuemei Hu and Daoyu Hu contributed to the development of the protocol, abstracted data, drafted and revised the abstract. All authors are in agreement with the content of the abstract.References
1. Siegel RL, Miller KD, Fedewa SA, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin 2017.
2. Tripathi P, Rao SX, Zeng MS. Clinical value of MRI-detected extramural venous invasion in rectal cancer. J Dig Dis 2017;18:2-12.
3. Zhang X-Y, Wang S, Li X-T, et al. MRI of Extramural Venous Invasion in Locally Advanced Rectal Cancer: Relationship to Tumor Recurrence and Overall Survival. Radiology 2018;289:677-685.
4. Yoo HY, Shin R, Ha H-K, et al. Does t3 subdivision correlate with nodal or distant metastasis in colorectal cancer? J Korean Soc Coloproctol 2012;28:160-164.
5. Vukobrat-Bijedic Z, Husic-Selimovic A, Sofic A, et al. Cancer Antigens (CEA and CA 19-9) as Markers of Advanced Stage of Colorectal Carcinoma. Med Arch (Sarajevo, Bosnia Herzegovina) 2013;67:397-401.
6. Kim JS, Sohn DK, Park JW, et al. Prognostic significance of distribution of lymph node metastasis in advanced mid or low rectal cancer. J Surg Oncol 2011;104:486-492.
7. Zhou Y, Wang H, Gong H, Cao M, Zhang G, Wang Y. Clinical significance of perineural invasion in stages II and III colorectal cancer. Pathol Res Pr 2015;211:839-844.
8. Bianchini F, Kaaks R, Vainio H. Overweight, obesity, and cancer risk. Lancet Oncol 2002;3:565-574.
9. Maurer CA, Renzulli P, Kull C, et al. The impact of the introduction of total mesorectal excision on local recurrence rate and survival in rectal cancer: long-term results. Ann Surg Oncol 2011;18:1899-1906.
10. Fiorica F, Cartei F, Licata A, et al. Can chemotherapy concomitantly delivered with radiotherapy improve survival of patients with resectable rectal cancer? A meta-analysis of literature data. Cancer Treat Rev 2010;36:539-549.
11. Nagtegaal ID, van de Velde CJH, Marijnen C a M, van Krieken JHJM, Quirke P. Low rectal cancer: a call for a change of approach in abdominoperineal resection. J Clin Oncol 2005;23:9257-9264.
12. Halappa VG, Villalobos CPC, Bonekamp S, et al. Rectal imaging: Part 1, high-resolution MRI of carcinoma of the rectum at 3 T. Am J Roentgenol 2012;199.
13. Tripathi P, Guo W, Rao S, Zeng M, Hu D. Additional value of MRI-detected EMVI scoring system in rectal cancer: applicability in predicting synchronous metastasis. Tumori 2020;106:286-294.
14. Cheng L-J, Chen J-H, Chen S-Y, et al. Distinct Prognosis of High Versus Mid/Low Rectal Cancer: a Propensity Score-Matched Cohort Study. J Gastrointest Surg January 2019.
15. Gu C, Yang X, Zhang X, et al. Clinical significance of the EMD/mesorectum ratio of T3 mid-low rectal cancer: A retrospective observational study. Medicine (Baltimore) 2018;97:e13468-e13468.
16. Shen L, Sun Y, Zhang H, et al. T3 subclassification using the EMD/mesorectum ratio predicts neoadjuvant chemoradiation outcome in T3 rectal cancer patients. Br J Radiol 2018;91:20170617.
17. Battersby NJ, How P, Moran B, et al. Prospective Validation of a Low Rectal Cancer Magnetic Resonance Imaging Staging System and Development of a Local Recurrence Risk Stratification Model: The MERCURY II Study. Ann Surg 2016;263:751-760.
18. Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol 2008;26:303-312.
19. Sueda T, Ohue M, Noura S, Shingai T, Nakanishi K, Yano M. Prognostic significance of a preoperative magnetic resonance imaging assessment of the distance of mesorectal extension in clinical T3 lower rectal cancer. Surg Today 2016;46:1249-1257.
20. Pratik T, Guo W, Yang C, Bimal R, Zeng M. Clinical feasibility assessment of T3 sub-stage in rectal cancer using MRI. Iran J Radiol 2018;15.
21. Cho SH, Kim SH, Bae JH, et al. Prognostic stratification by extramural depth of tumor invasion of primary rectal cancer based on the Radiological Society of North America proposal. Am J Roentgenol 2014;202:1238-1244.
22. Tong T, Sun Y, Cai S, Zhang Z, Gu Y. Extramural depth of rectal cancer tumor invasion at thin-section MRI: predicting treatment response to neoadjuvant chemoradiation. Oncotarget 2015;6:30277-30286.
23. de’Angelis N, Pigneur F, Martinez-Perez A, et al. Assessing surgical difficulty in locally advanced mid-low rectal cancer: the accuracy of two MRI-based predictive scores. Colorectal Dis 2019;21:277-286.
24. Escal L, Nougaret S, Guiu B, et al. MRI-based score to predict surgical difficulty in patients with rectal cancer. Br J Surg 2018;105:140-146.
25. Boyle KM, Chalmers AG, Finan PJ, Sagar PM, Burke D. Morphology of the mesorectum in patients with primary rectal cancer. Dis Colon Rectum 2009;52:1122-1129.
26. Allen SD, Gada V, Blunt DM. Variation of mesorectal volume with abdominal fat volume in patients with rectal carcinoma: assessment with MRI. Br J Radiol 2007;80:242-247.
27. Yamaoka Y, Yamaguchi T, Kinugasa Y, et al. Mesorectal fat area as a useful predictor of the difficulty of robotic-assisted laparoscopic total mesorectal excision for rectal cancer. Surg Endosc 2019;33:557-566.
28. Yoon J, Chung YE, Lim JS, Kim M-J. Quantitative assessment of mesorectal fat: new prognostic biomarker in patients with mid-to-lower rectal cancer. Eur Radiol 2019;
29:1240-1247.29. Pooni A, Al-Sukhni E, Milot L, et al. Selection of Patients With Rectal Cancer for Preoperative Chemoradiotherapy: Are T Category and Nodal Status All That Matters? Dis Colon Rectum 2019;62:447-453.
30. Glynne-Jones R, Wyrwicz L, Tiret E, et al. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol Off J Eur Soc Med Oncol 2018;29:iv263.
31. Benson AB, Venook AP, Al-Hawary MM, et al. Rectal Cancer, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2018;16:874-901.
32. Wang J, Thornton JC, Russell M, Burastero S, Heymsfield S, Pierson RNJ. Asians have lower body mass index (BMI) but higher percent body fat than do whites: comparisons of anthropometric measurements. Am J Clin Nutr 1994;60:23-28.
33. Wong EMF, Lai BMH, Fung VKP, et al. Limitation of radiological T3 subclassification of rectal cancer due to paucity of mesorectal fat in Chinese patients. Hong Kong Med J = Xianggang yi xue za zhi 2014;20:366-370.
Figures
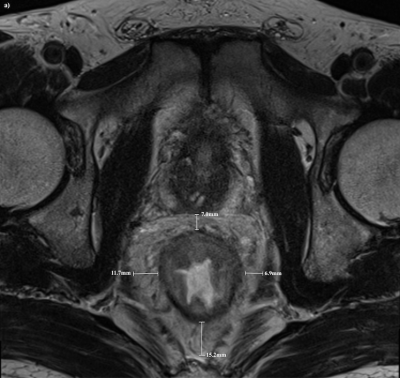
Title: Axial view of mesorectum using MRI
Legend: Axial view of anterior, posterior, right lateral and left lateral mesorectal fat thickness at the level of 5 cm from the anal verge
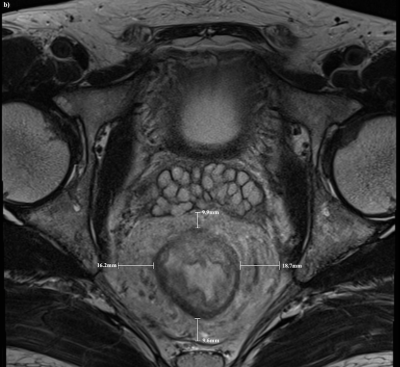
Title: Axial view of mesorectum using MRI
Legend: Axial view of anterior, posterior, right lateral and left lateral mesorectal fat thickness at the level of 5 cm from the anal verge
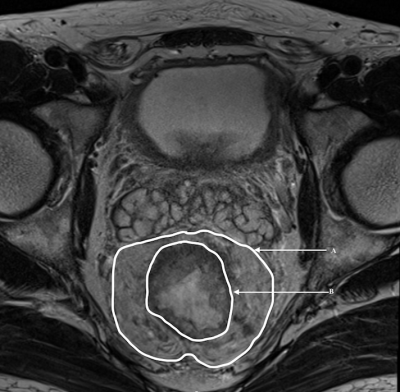
Title: Axial view of mesorectal fat thickness using MRI
Legend: The mesorectal fat area was calculated by subtracting the rectal area (inner circle, B) from the mesorectal area (outer circle, A) on axial T2-weighted image