0353
Maternal Obesity during Pregnancy is Associated with Lower Cortical Thickness in the Newborn Brain
Xiaoxu Na1, Natalie E. Phelan1, Marinna R. Tadros1, Aline Andres2,3, Thomas M. Badger2,3, Charles M. Glasier1, Raghu H. Ramakrishnaiah1, Amy C. Rowell1, Li Wang4, Gang Li4, Zhengwang Wu4, David K. Williams5, and Xiawei Ou1,3,6
1Radiology, University of Arkansas for Medical Sciences, Little Rock, AR, United States, 2Pediatrics, University of Arkansas for Medical Sciences, Little Rock, AR, United States, 3Arkansas Children's Nutrition Center, Little Rock, AR, United States, 4Radiology, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States, 5Biostatistics, University of Arkansas for Medical Sciences, Little Rock, AR, United States, 6Arkansas Children's Research Institute, Little Rock, AR, United States
1Radiology, University of Arkansas for Medical Sciences, Little Rock, AR, United States, 2Pediatrics, University of Arkansas for Medical Sciences, Little Rock, AR, United States, 3Arkansas Children's Nutrition Center, Little Rock, AR, United States, 4Radiology, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States, 5Biostatistics, University of Arkansas for Medical Sciences, Little Rock, AR, United States, 6Arkansas Children's Research Institute, Little Rock, AR, United States
Synopsis
This study examined the relationships between maternal obesity during pregnancy and newborn’s brain cortical development. Healthy normal weight or obese pregnant women were recruited at early pregnancy and their newborns underwent a brain MRI examination at 2 weeks of age. Structural MR images of the brain were post-processed to reconstruct cortical surfaces, and mean cortical thickness in different brain regions was measured. Significant differences in cortical thickness between infants born to normal weight vs. obese mothers were found in multiple brain regions, and negative correlations between maternal body fat mass percentage and infant cortical thickness were also observed.
INTRODUCTION
Obesity during pregnancy is a prevalent health concern, not only for the pregnant women, but also for their offspring. Recent studies have suggested that maternal obesity is associated with changes in cognitive and neurodevelopmental outcomes in children. Nevertheless, little is known why there are such associations. Imaging the developing brain soon after birth provides an opportunity to detect potential disruptions in fetal brain development associated with maternal obesity, and to link them with changes in neurodevelopmental outcomes. In this study, we aimed at investigating relationships between maternal obesity during early pregnancy and newborn brain cortical development. Our hypothesis was that maternal obesity during pregnancy would slow down fetal cortical development and this can be reflected by lower newborn cortical thickness in different brain regions.METHODS
Healthy pregnant women and their newborn infants were recruited for this prospective study. Inclusion criteria for the pregnant women were: pre-pregnancy BMI 18.5-24.9 (normal weight group) or 30-35 (obese group); second parity, singleton pregnancy; ≥21 years of age; conceived without assisted fertility treatments. Exclusion criteria for the pregnant women were: pre-existing medical conditions such as diabetes mellitus, seizure disorder, and serious psychiatric disorders; drug or alcohol abuse; sexually transmitted diseases; medical complications during pregnancy such as gestational diabetes and pre-eclampsia. In addition, infants born pre-term (<37 weeks of gestation) or with medical conditions or medications known to influence growth and development, or unable to complete MRI without sedation (N=2) were also excluded. In total, 44 pregnant women (28 normal weight, 16 obese) and their infants completed the experimental procedures and were included in this study. All pregnant women had their body composition assessed using air displacement plethysmography and BMI measured at 12 weeks of pregnancy. Maternal IQ was also assessed using the Wechsler Abbreviated Scale of Intelligence. After the birth of their newborns, birth weight and length were retrieved from medical records. At 14±2 days, the newborns underwent an MRI examination of the brain during natural sleep without sedation. A neonatal MRI protocol was used, and all images were exported to the local PACS system and were screened for incidental findings. In addition, 3D T1-weighted images with resolution of 1mm x 1mm x 1mm were post-processed by iBEAT V2.0 software (developed by the Developing Brain Computing lab and Baby Brain Mapping lab at the University of North Carolina at Chapel Hill) to reconstruct for cortical surface and to measure cortical thickness. Specifically, 3D T1-weighted MR images were corrected for inhomogeneity before skull stripping, followed by tissue segmentation, left/right hemisphere separation, topology correction and inner/outer cortical surfaces reconstruction. Cortical thickness between infants born to normal-weight or obese mothers were compared using ANOVA with covariates of infant sex, postmenstrual age at MRI (gestational length at birth plus postnatal days at MRI), maternal age at pregnancy, and maternal IQ, for 68 cortical regions defined by the Desikan atlas. False discovery rate (FDR) correction was used for multiple comparison correction, and regions with FDR corrected P values < 0.05 were regarded as significantly different in cortical thickness between groups. Additionally, for those regions identified by ANOVA, Spearman’s rank partial correlation tests were used to evaluate relationships between maternal body fat mass percentage and infant brain cortical thickness.RESULTS
The ANOVA analysis showed that there were 3 cortical regions with significant differences (FDR corrected P < 0.05) in mean cortical thickness between infants born to normal weight vs. obese pregnant women (Figure 1). Specifically, the mean cortical thickness was higher in infants born to normal weight vs. obese pregnant women in the left pars opercularis gyrus (1.99 ± 0.07 mm vs. 1.90 ± 0.07 mm, FDR corrected P = 0.009); the left pars triangularis gyrus (1.92 ± 0.07 mm vs. 1.84 ± 0.06 mm, FDR corrected P = 0.02); and the left rostral middle frontal gyrus (1.78 ± 0.03 mm vs. 1.74 ± 0.04 mm, FDR corrected P = 0.02).Furthermore, significant negative correlations (P < 0.05, controlled for same covariates as in the ANOVA analysis) between maternal body fat mass percentage and infant brain cortical thickness were observed in all of these 3 regions (Figure 2).
CONCLUSIONS
Our results indicate that maternal obesity during early pregnancy is associated with lower cortical thickness in several brain regions in the left frontal lobe of newborn infants.Acknowledgements
This project was supported by NIH R01HD099099 and USDA/ARS 6026-51000-010-00-D.References
No reference found.Figures

Figure 1: The anatomical locations for the 3 brain cortical regions
that showed significant differences (FDR corrected P < 0.05) in mean
cortical thickness between infants born to normal weight vs. obese pregnant
women: a) the left pars opercularis (LPO) gyrus; b) the left pars triangularis
(LPT) gyrus; and c) the left rostral middle frontal (LRMF) gyrus. The
comparison of mean cortical thickness for these 3 regions between these two
groups of infants is illustrated in d).
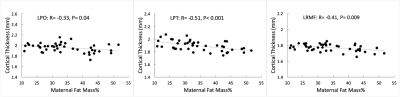
Figure 2:
Partial correlation analysis showed significant negative correlations (P <
0.05) between maternal body fat mass percentage measured at ~12 weeks of
pregnancy and infant brain mean cortical thickness measured at ~2 weeks of
postnatal age in the a) left pars opercularis (LPO) gyrus; b) left pars
triangularis (LPT) gyrus; and c) left rostral middle frontal (LRMF) gyrus.