0349
Clinical fetal cardiovascular MRI based on Doppler ultrasound gating at 3T and 1.5T: On a technical aspect of imaging pulse sequence optimization1Philips, Hamburg, Germany, 2Department of Diagnostic and Interventional Radiology and Nuclear Medicine, University Hospital Hamburg-Eppendorf, Hamburg, Germany, 3Department of Biomedical Imaging and Image-Guided Therapy, Division of Neuroradiology and Musculoskeletal Radiology, Medical University of Vienna, Vienna, Austria, 4Department of Obstetrics and Fetal Medicine, University Hospital Hamburg-Eppendorf, Hamburg, Germany, 5Department of Gynecology and Obstetrics, Division of Feto-Maternal Medicine, Medical University of Vienna, Vienna, Austria, 6northh medical GmbH, Hamburg, Germany
Synopsis
Cardiovascular MRI is considered a valuable diagnostic tool for studying congenital abnormalities in children and adults. However, simple, high-quality imaging of the fetal heart is challenging due to lack of direct in-utero cardiac gating. We aimed to employ a recently introduced Doppler ultrasound (DUS) device and combine with optimized routine imaging techniques for structural and functional studies of the fetal heart and to establish a standard acquisition approach for high-quality fetal cardiovascular MRI in the clinical practice.
Introduction
Magnetic resonance imaging of the cardiovascular system is considered a valuable diagnostic tool for studying congenital or development abnormalities in children and adults. However, simple, high-quality imaging of the fetal heart is challenging due to lack of direct in-utero cardiac gating. We aimed to employ a recently introduced Doppler ultrasound (DUS) device 1-2 and optimized pulse sequences for structural and functional imaging of the fetal heart and to establish a standard acquisition approach for high-quality fetal cardiovascular MRI in the clinical practice.Methods
All pregnant women with or without previously diagnosed or suspected heart malformations in prenatal ultrasound underwent fetal cardiovascular MRI on 3.0T or 1.5T clinical whole-body systems (Ingenia, Philips Healthcare, Best, the Netherlands) with 70 cm bore and a standard 32-channel torso coil. Subjects were examined in either supine or lateral decubitus position. A MR-compatible DUS device was used to sense the fetal cardiac motion and generate signals for MR image acquisition with direct fetal cardiac gating 1-2. Imaging pulse sequences for cardiovascular structural and functional exams were adapted from conventional protocols and these included:- Survey (i.e. localization or scout scan) based on multi-planar gradient-echo sequences without cardiac gating
- Morphological exam based on single-shot turbo-field echo with balanced steady-state free precession (bTFE or bSSFP) or single-shot turbo-spin echo (TSE) sequences, in orthogonal orientations
- Functional exam based on multi-shot bTFE cine sequences with cardiac gating
- 4D flow based on phase-contrast velocity-encoded turbo-field echo (TFE) sequences with cardiac gating
- Native myocardial T1 mapping based on Modified Look-Locker Imaging (MOLLI) with cardiac-triggered single-shot bTFE
Results and Discussion
Nine fetuses were studied (gestational age 30 to 36 weeks). Fetal cardiac frequency ranged from 130 to 180 beats per minute (bpm). All data were successfully acquired with DUS gating. Two patients were excluded from analysis due to severe fetal movement.Figure 1 demonstrated a typical optimization process from single-shot non-gated bTFE without gating to multi-shot bTFE cine with DUS fetal cardiac gating for better delineation of the cardiac motions. Imaging times of functional cine exams were typically 7 to 12 s for BH scans and 30 to 40 s for FB scans with multiple averaging (NSA = 3 to 4) to mitigate gross motion without respiratory navigator. Different anatomical orientations including 4-chamber and short-axis cardiac views showed good image quality with excellent myocardium-to-blood contrast and clear fetal myocardial contractions in both sequence setups. Typical case examples on 1.5T and 3.0T were shown in Figure 1 and 2. No significant difference was found between BH and FB scans under shallow and regular maternal breathing. Otherwise, BH scans were deemed better with clearly less motion-induced aliasing artifacts.
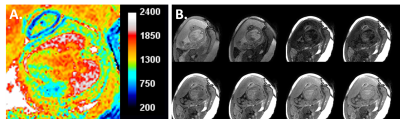
Fetal circulation could be visualized in 4D flow, showing ductus arteriosus (DA) connecting the trunk of the pulmonary artery to the proximal descending aorta (AoD), which allows blood from the right ventricle to bypass the fetus's fluid-filled non-functioning lungs (Figure 3). Blood flow in the ductus was seen with high velocities, which mixed with the blood from the ascending aorta and created spiral-shape vortices that were also clearly visible in AoD. Quantitative flow measurements in AoD were in accordance to the previous reports 3-4 (results not shown here). T1 maps could be obtained and ROI analysis from the inter-ventricular septum revealed a mean native myocardium T1 of 1090 ± 69 ms (Figure 4). In certain cases image registration may help to further compensate residual motion in post-processing, as in the adult case 5.
Conclusion
Fetal cardiovascular MRI was possible based on direct fetal cardiac gating from the DUS device. The benefits have been demonstrated with promise in high-quality morphological and functional studies of the fetal heart using routinely available imaging techniques. Preliminary experience in patients with free breathing may further foresee a wide clinical adoption for evaluation of congenital pathologies. Future studies are warranted to investigate its robustness and clinical performance.Acknowledgements
The authors thank Dr. Hendrik Kooijman-Kurfuerst for his help in preparation of the scan protocols.References
- Kording F, et al. J Cardiovas Magn Reson (2018) 20:17.
- Kording F, et al. Magn Reson Med Sci (2018) 17:308.
- Schoennagel BP, et al. Eur Radiol (2019) 29:4169.
- Salehi D, et al. J Cardiovasc Magn Reson (2019) 21:74.
- Zhang S, et al . Proc ISMRM, Honolulu (2017) 25:2754.
Figures
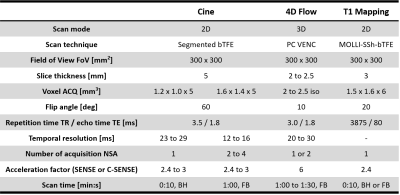
Table 1. Imaging pulse sequences using Doppler ultrasound (DUS) for fetal cardiac gating. The main parameters were kept comparable between 3.0T and 1.5T. See text for scan protocols used in this study.
bTFE = balanced turbo-field echo; PC = phase contrast; VENC = velocity encoded; SSh = single shot; MOLLI = Modified Look-Locker Imaging; ACQ = acquired; SENSE = sensitivity encoding; C-SENSE = compressed SENSE
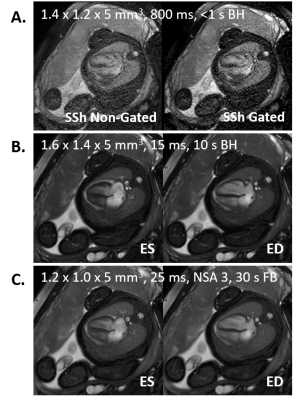
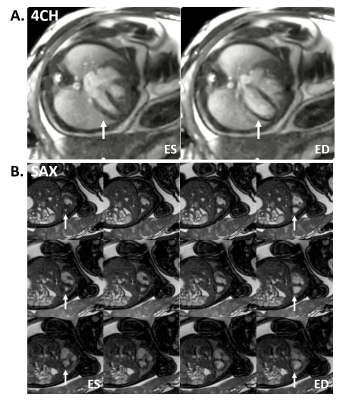
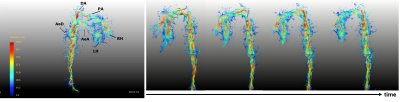
Figure 3. 4D flow exam of the fetal heart based on DUS fetal cardiac gating. Image examples with streamline visualization were selected from a case at 35 gestational weeks on 3.0T. Details see text.
DA = ductus arteriosus; PA = pulmonary artery; AoD = descending aorta; AoA = ascending aorta; RH = right heart; LH = left heart