0308
Sildenafil Administration Improves Right Ventricular Function on 4D Flow MRI in Young Adults Born Premature1University of Wisconsin-Madison, Madison, WI, United States, 2University of Texas Southwestern, Dallas, TX, United States, 3Mayo Clinic, Rochester, MN, United States
Synopsis
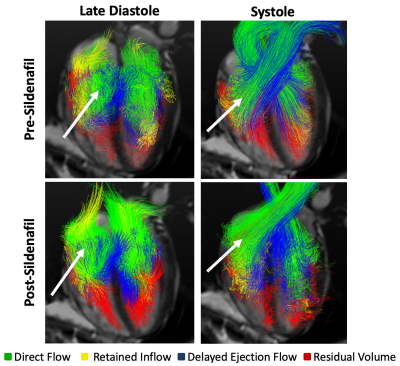
We used 4D flow MRI before and during acute pharmacological intervention to reduce either afterload or heart rate in young adults born very to extremely premature, finding improved overall cardiac function and shifted intraventricular flow in the RV towards direct flow after RV afterload reduction with sildenafil. We interpret these findings to mean that intrinsic morphologic differences as well as increased RV afterload are stronger drivers of cardiac dysfunction in the preterm heart than decreased filling time. This study design may serve as a blueprint for future studies investigating the effects of acute hemodynamic pharmacological interventions with 4D flow MRI.
INTRODUCTION
As advances in the treatment of extremely premature infants decrease mortality1, the long-term ramifications of premature birth are coming to light. In addition to known pulmonary consequences of premature birth, recent evidence suggests an up to 17-fold increased risk of heart failure in those born extremely premature (≤28 gestational weeks)2. Imaging studies have investigated cardiac structural and functional differences in young adults born premature compared to term-born controls, finding smaller biventricular chambers and stroke volumes3. Functionally, the right ventricle (RV) appears to be more affected. RV dysfunction4 and pulmonary hypertension5 has been identified in young adults born preterm. Individuals born premature frequently have higher resting heart rates (HR) which may also contribute to dysfunction via impaired filling time. In order to investigate these two mechanisms, we used acute pharmacological interventions, coupled with 4D flow MRI – a technique to measure 3-directional blood flow in a volumetric region in-vivo—in order to measure intracardiac flow patterns before and after the interventions. Specifically, we studied the effects of RV afterload reduction and HR reduction, representing a novel use of 4D flow MRI to measure acute intraventricular hemodynamic effects of cardiac-targeted therapeutics.METHODS
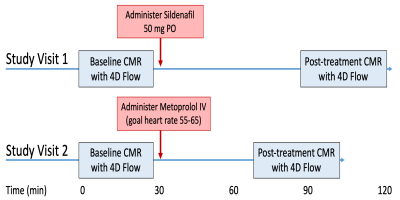
Nine young adults (3M/6F) born very to extremely premature (gestational age ≤32 weeks or birth weight <1500g) participated in this study, which used a crossover design with each participant undergoing 2 visits (Figure 1). On the first visit, each subject was randomized to receive either intravenous metoprolol tartrate (Lopressor; Novartis Pharmaceuticals Corporation; East Hanover, NJ, USA; titrated to achieve a HR of 55-65), a beta-blocker, or oral sildenafil citrate (Viagra; Pfizer; New York, NY, USA; 50mg), a pulmonary vasodilator. Each subject received the other drug on the second visit. Each subject underwent cardiac MRI on a 3T scanner (Signa Premier, GE Healthcare, Waukesha, WI) with a 30-channel phased-array flexible coil both before and after drug administration. Scans included breath-held short-axis cine balanced steady-state free precession (bSSFP) imaging (TR/TE=3.1/1.1ms, field of view=40x40cm, acquired spatial resolution=1.79x1.79mm, slice thickness=8mm, reconstructed cardiac phases=20) and 4D flow cardiac MRI (acquired with radially undersampled sequence [PC VIPR6]; velocity encoding=150cm/s, acquired spatial resolution=2.5mm isotropic, acquired & reconstructed cardiac phases=20). The left ventricle (LV) and RV cavities were manually segmented at each time frame on bSSFP images using Segment7 (Medviso, version 2.2 R6423; http://segment.heiberg.se). The contours were used to compute ventricular volumes and function. The short axis dataset was then rigidly registered (using ANTs8) to the 4D flow time-averaged magnitude image, and ventricular velocities were extracted from endocardial segmentations for flow analysis9. The distribution of different ventricular flow components was determined in all subjects using the method of Eriksson et al10. Blood pathlines were emitted from the blood volume of each ventricle and traced forwards and backwards in time over one cardiac cycle. Pathlines were sorted into four components: direct flow, retained inflow, delayed ejection flow, and residual volume. Paired-sample Wilcoxon signed rank tests were then used to determine significant changes in CMR parameters with each drug administration.RESULTS
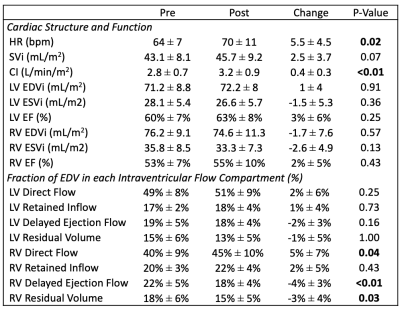
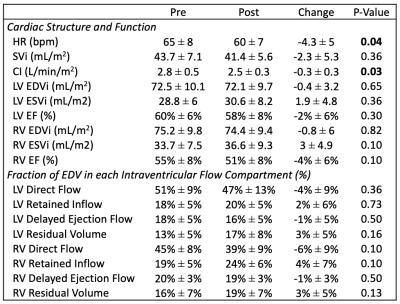
Average gestational age, birth weight, and chronological age were 28.9 ± 2.7 weeks, 1120 ± 340 g, and 27.8 ± 3.7 years, respectively. Standard measures of cardiac morphometry and function on the sildenafil day (Table 1) revealed a 14% increase in cardiac index, mediated by a 9% increase in HR and 6% increase in stroke volume index. Flow compartment analysis of 4D flow MRI data (Figure 2) revealed a significant shift towards direct flow in the RV, with a 13% increase in RV direct flow fraction and a 17% decrease in RV residual volume fraction. Standard measures of cardiac morphometry and function on the Metoprolol day (Table 2) revealed an 11% decrease in cardiac index, mediated by a 7% decrease in HR and 5% decrease in stroke volume. No significant changes in flow compartment distribution resulted from Metoprolol administration.DISCUSSION
In this study, we aimed to determine the effect of afterload reduction and heart rate reduction on cardiac hemodynamics and function using 4D flow MRI during pharmacological intervention. We found that RV afterload reduction with sildenafil improved overall cardiac function and shifted intraventricular flow in the RV towards direct flow. On the other hand, metoprolol reduced cardiac index without affecting intraventricular flow compartment distribution. We interpret these findings to mean that intrinsic morphologic differences as well as increased RV afterload5 are stronger drivers of cardiac dysfunction in the preterm heart than decreased filling time. Further, the smaller biventricular cavity size signifies that the preterm heart is likely less able to augment stroke volume and considerably more heart rate dependent at baseline.CONCLUSION
We used 4D flow MRI before and during pharmacological intervention to reduce either afterload or heart rate, finding improved overall cardiac function and shifted intraventricular flow in the RV towards direct flow after RV afterload reduction with sildenafil. This study design may serve as a blueprint for future studies investigating the effects of acute hemodynamic pharmacological interventions with 4D flow MRI. Whether long-term sildenafil administration may improve ventricular-vascular interactions in high-risk preterm-born individuals merits further study.Acknowledgements
Kara Goss is supported by the University of Wisconsin Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant NIH UL1TR000427 (Primary investigator Marc Drezner; 4KL2TR000428-10), as well as a Parker B Francis Fellowship Award and American Heart Association Career Development Award (Goss, #18CDA34110440). Philip A Corrado is supported by the National Heart, Lung, And Blood Institute of the NIH under Award Number F31HL144020. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We gratefully thank GE Healthcare for MRI research support.References
1. Younge N, Smith PB, Gustafson KE, et al. Improved survival and neurodevelopmental outcomes among extremely premature infants born near the limit of viability. Early Hum Dev. 2016;95:5-8. doi:10.1016/j.earlhumdev.2016.01.015
2. Carr H, Cnattingius S, Granath F, Ludvigsson JF, Edstedt Bonamy AK. Preterm Birth and Risk of Heart Failure Up to Early Adulthood. J Am Coll Cardiol. 2017;69(21):2634-2642. doi:10.1016/j.jacc.2017.03.572
3. Goss KN, Haraldsdottir K, Beshish AG, et al. Association Between Preterm Birth and Arrested Cardiac Growth in Adolescents and Young Adults. JAMA Cardiol. 2020:1-10. doi:10.1001/jamacardio.2020.1511
4. Telles F, McNamara N, Nanayakkara S, et al. Changes in the Preterm Heart From Birth to Young Adulthood: A Meta-analysis. Pediatrics. 2020;146(2). doi:10.1542/peds.2020-0146
5. Goss KN, Beshish AG, Barton GP, et al. Early pulmonary vascular disease in young adults born preterm. Am J Respir Crit Care Med. 2018;198(12):1549-1558. doi:10.1164/rccm.201710-2016OC
6. Gu T, Korosec FR, Block WF, et al. PC VIPR: A high-speed 3D phase-contrast method for flow quantification and high-resolution angiography. Am J Neuroradiol. 2005;26:743-749. doi:26/4/743 [pii]
7. Heiberg E, Sjögren J, Ugander M, Carlsson M, Engblom H, Arheden H. Design and validation of Segment - freely available software for cardiovascular image analysis. BMC Med Imaging. 2010;10:1-13. doi:10.1186/1471-2342-10-1
8. Avants BB, Tustison NJ, Stauffer M, Song G, Wu B, Gee JC. The Insight ToolKit image registration framework. Front Neuroinform. 2014;8:1-13. doi:10.3389/fninf.2014.00044
9. Gupta V, Bustamante M, Fredriksson A, Carlhall CJ, Ebbers T. Improving left ventricular segmentation in four-dimensional flow MRI using intramodality image registration for cardiac blood flow analysis. Magn Reson Med. 2018;79(1):554-560. doi:10.1002/mrm.26674
10. Eriksson J, Carlhäll C, Dyverfeldt P, Engvall J, Bolger AF, Ebbers T. Semi-automatic quantification of 4D left ventricular blood flow. J Cardiovasc Magn Reson. 2010;12(1):9. doi:10.1186/1532-429X-12-9
Figures