0270
Tau correlates with tissue susceptibility and microstructure in APOE-ε4+ mild cognitive impairment1Center for Advanced Neuroimaging, University of California Riverside, Riverside, CA, United States, 2Department of Neurology, Emory University, Atlanta, GA, United States, 3Department of Bioengineering, University of California Riverside, Riverside, CA, United States, 4Department of Psychology, University of California Riverside, Riverside, CA, United States
Synopsis
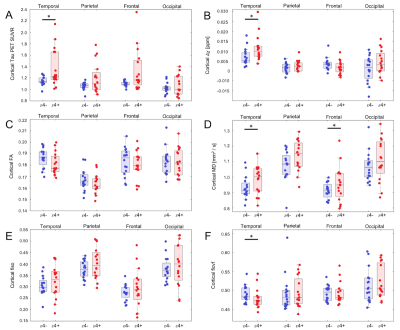
We examine the impact of APOE-ε4 carrier status on cortical iron, gray matter microstructure, and tau-PET signal in mild cognitive impairment. We found significant increases in susceptibility (p=0.01), tau-PET SUVR (p=0.01), and MD (p=0.046) in the temporal lobe of APOE-ε4 positive compared to APOE-ε4 negative participants. Significant correlations were seen between tau-PET SUVR and susceptibility (r=0.717), FA (r=-0.431), and MD (r=0.435) in the temporal lobe of APOE-ε4 positive participants. Taken together, these findings suggest that APOE-ε4 allele increases the risk of developing AD pathology and accumulating iron, which in turn leads to degradation of cortical tissue microstructure.
Introduction
Alzheimer’s disease (AD) is the most frequent cause of neurodegenerative dementia. Patients with mild cognitive impairment (MCI) exhibit declines in cognitive performance that do not meet the threshold for dementia, but are likely to later convert to AD1. AD and MCI pathology include the accumulation of β-amyloid (Aβ) into extracellular plaques and hyper-phosphorylated tau into intracellular neurofibrillary tangles2,3.Individuals carrying the apolipoprotein E-ε4 (APOE-ε4) allele are at increased risk of developing AD pathology4. This may be due to higher cortical iron burden5,6, which has also been linked to degradation of tissue microstructure7. Recent work has shown that tau-PET signal is correlated with cortical susceptibility values, which quantify iron burden in AD patients8. However, the impact of APOE-ε4 carrier status on cortical iron, gray matter microstructure, and tau-PET signal is largely unexplored in MCI. These relationships were examined here in APOE-ε4 positive (i.e. one or more APOE-ε4 alleles) and APOE-ε4 negative MCI patients.
Methods
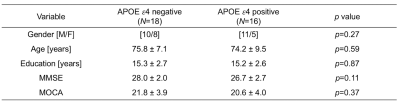
The Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu) was queried for individuals diagnosed with MCI who had APOE-ε4 data, tau-sensitive PET (18F-AV1451), multi-echo gradient echo MRI images, and two shell diffusion MRI data acquired at the same visit. MCI diagnoses were based on a subjective memory concern reported by a clinician, abnormal memory function on the education-adjusted Logical Memory II subscale, and a clinical dementia rating greater than 0.5. A total of 34 MCI participants met these criteria. Participants with either one or two APOE-ε4 alleles were considered APOE-ε4 (+). Demographic information is shown Table 1.All MRI data were acquired on Siemens Prisma scanners. Anatomic images were acquired with a T1-weighted MP-RAGE sequence (echo time (TE)/repetition time (TR)/inversion time=2.98/2300/900 ms, flip angle=9°, voxel size=1.0×1.0×1.0 mm3) and were used for registration to common space and correction of partial volume effects in the PET data.
Multi-echo data were collected with a 2D gradient recalled echo sequence (TE1/∆TE/TR=6/7/650 ms, voxel size=0.86×0.86×4 mm3, 44 slices). R2* and quantitative susceptibility maps (QSM) images were calculated in MATLAB.
Diffusion tensor imaging (DTI) data were acquired with a multiband diffusion weighted EPI spin echo sequence (TE/TR=71/3400ms, voxel size=2×2×2mm3). Diffusion weighting was applied in 54 directions with b values of 1000 and 2000 s/mm2. DTI data were first corrected for motion and eddy currents using eddy in FSL. Next, susceptibility distortions were corrected using fugue. Neurite orientation and dispersion density imaging (NODDI) metrics were calculated in MATLAB using the NODDI toolbox v1.0.1.
18F-AV1451 PET (tau-PET) imaging was performed at each ADNI site according to standardized protocols. The 18F-AV-1451 protocol entailed injection of 10 mCi of tracer followed by an uptake phase of 80 min during which the subjects remained out of the scanner. 18F-AV-1451 emission data were collected as 4×5min frames. PET imaging data were analyzed with FSL and PET partial volume correction (PETPVC) toolbox. 18F-AV1451 PET scans were motion corrected, averaged, registered to the participant's own T1-weighted MRI image. Grey matter, white matter, and CSF maps were segmented in the T1-weighted image and used to correct for partial volume effects. The median standardized uptake value (SUV) in the inferior cerebellar cortex was chosen as a reference and used to calculate mean SUV ratio (SUVR) in cortical ROIs. Figure 1 shows typical SUVR and susceptibility maps in an APOE-ε4 positive subject.
For each of four cortical lobe regions of interest (ROIs; temporal, parietal, frontal, occipital), we measured mean diffusion (FA, fractional anisotropy; mean diffusivity, MD), NODDI (fiso, ficvf, odi), susceptibility, and tau-PET (SUVR) metrics.
Results
In the temporal lobe, significant increases in susceptibility (p=0.01), tau-PET SUVR (p=0.01), and MD (p=0.046) were observed for APOE-ε4 positive compared to APOE-e4 negative participants, with trends for decreased temporal lobe FA (p=0.055) and the intra-cellular compartment volume fraction (ficvf; p=0.047). In the frontal lobe, significant increases in tau-PET SUVR (p=0.03) and MD (p=0.02) were seen in APOE-ε4 positive participants, with a trend toward decreased FA (p=0.08) and increased susceptibility (p=0.09). No other cortical regions exhibited significant group differences. These comparisons are summarized in Figure 2.Post hoc correlations between tau-PET SUVR and MRI measures in the temporal lobe were assessed using Spearman’s rank correlations, separately for each APOE-ε4 status. Interestingly, significant correlations were seen between tau-PET SUVR and susceptibility (r=0.717), FA (r=-0.431), and MD (r=0.435) in the temporal lobe of APOE-ε4 positive participants. However, no significant correlations were seen between tau-PET SUVR and any MRI measure (susceptibility:r=0.245; MD:r=-0.287; FA:r=0.167 ) in the temporal lobe in APOE-ε4 negative participants.
Discussion
We found evidence of increased tau pathology (tau-PET SUVR), iron burden (susceptibility), and microstructural degradation (increased MD, decreased FA) in the temporal lobe of APOE-ε4 positive as compared to APOE-ε4 negative MCI participants. Interestingly, higher tau pathology in the temporal lobe was significantly related to multiple MRI metrics, but only in APOE-ε4 positive participants. In particular, higher cortical tau burden was correlated with diffusion metrics associated with neurodegeneration, which agrees with earlier work showing that tau uptake is also related to cortical thinning in AD9,10,11. Taken together, these findings suggest that APOE-ε4 allele increases the risk of developing AD pathology and accumulating iron, which in turn leads to degradation of cortical tissue microstructure.Acknowledgements
Data collection and sharing for this project was funded by the Alzheimer's Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.References
[1] Albert, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 7:270–279.
[2] Morris, et al. APOE predicts amyloid-beta but not tau Alzheimer pathology in cognitively normal aging. Ann Neurol 67:122-131.
[3] Schmechel, et al. Increase amyloid beta-peptide deposition in cerebral cortex as a consequence of apolipoprotein E genotype in late-onset Alzheimer disease. Proc Natl Acad Sci USA 90:9649-0653.
[4] Roses and Saunders. APOE is a major susceptibility gene for Alzheimer's disease. Curr Opin Biotechnol. 5:663-667.
[5] Wood. Alzheimer disease: Iron-the missing link between ApoE and Alzheimer disease? Nat. Rev Neurol. 11:369.
[6] Spotorno, et al. Relationship between cortical iron and tau aggregation in Alzheimer’s disease. Brain. 143:1341-1349.
[7] Bartzokis, et al. Apolipoprotein E affects both myelin breakdown and cognition: implications for age-related trajectories of decline into dementia. Biol Psychiatry. 62:1380–1387.
[8] Brier, et al. Tau and Ab imaging, CSF measures, and cognition in Alzheimer’s disease. Sci Transl Med. 8:338ra66.
[9] Iaccarino, et al. Local and distant relationships between amyloid, tau and neurodegeneration in Alzheimer's disease. Neuroimage Clin. 17:452–464.
[10] Xia, et al. Association of in Vivo [18F]AV-1451 tau PET imaging results with cortical atrophy and symptoms in typical and atypical Alzheimer disease. JAMA Neurol. 74:427–436.
[11] Sintini, et al. Regional multimodal relationships between tau, hypometabolism, atrophy, and fractional anisotropy in atypical Alzheimer's disease. Hum. Brain Mapp. 40:1618–1631.
Figures