0255
Optimizing T2-weighted MRI and DWI of the Esophagus1Radiology, University of Wisconsin-Madison, Madison, WI, United States, 2Global MR Applications and Workflow GE Healthcare, Madison, WI, United States, 3Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 4Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 5Medicine, University of Wisconsin-Madison, Madison, WI, United States, 6Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States
Synopsis
Esophageal MRI is emerging alternative to endoscopic ultrasound (EUS) and computed tomography (CT) for the detection and staging of cancer. Esophageal MRI has great potential for screening, active surveillance post-neodjuvant therapy and ruling out surgery for patients with higher stage cancer. The major challenges in esophageal imaging are the spatial resolution, as the esophageal wall is only approximately 3mm thick, and cardiac related motion artifacts. This prospective study aimed to address these challenges by developing a protocol for high-resolution T2-weighted and motion-robust diffusion-weighted imaging of the esophagus and periesophageal tissue.
Introduction
Esophageal cancer is the 7th most common cause of cancer and the 6th most common cause of cancer death, worldwide1. Currently, the combination of endoscopic ultrasound (EUS), computed tomography (CT) and positron emission tomography (PET)-CT are used for locoregional staging and disease management. Few MRI studies have shown promising results in determination of tumor stage and therapy response2–4. While T2-weighted (T2w) MRI imaging allows for morphological assessment of the esophageal wall and lesions5, diffusion weighted imaging (DWI) and its associated apparent diffusion coefficient (ADC), may enable esophageal tissue assessment quantitatively6.However, both T2w and DWI are limited by spatial resolution as the esophageal wall is only approximately 3mm thick. Furthermore, motion artifacts diminish image quality, and may lead to bias in DWI measurements. Cardiovascular-related motion effects in DWI may not be avoidable through gating or respiratory triggering, leading to unpredictable signal loss in DWI due to the motion sensitivity of standard (‘monopolar’) diffusion gradient waveforms used in DWI. Recently, optimized motion-compensated gradient waveforms have been proposed to address these artifacts7,8, with the potential to enable repeatable and reliable ADC measurements.
Improvements in T2w and DWI, may increase MRI value for screening and disease management of esophageal cancer. Therefore, the purpose of this study was to develop a multiparametric MRI protocol in vivo, with high-resolution T2w and motion-robust DWI.
Methods
This prospective study was performed with Institutional Review Board approval. Five healthy volunteers (mean age 33 years, range 29-37 years; 4 males/1 female; mean BMI 23.1, range 20.5-26.6) were imaged at 3T (Signa Premier, GE Healthcare, Waukesha, WI) using an external 30 channel phased-array (AIR Coil, GE Healthcare) with posterior elements embedded in the scanner table.Images were acquired and evaluated in the lower esophagus and esophagogastric junction. The study goals were to:
1. Maximize spatial resolution of T2w images by adjustment of acquisition parameters.
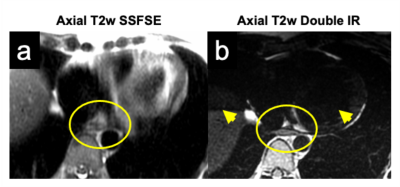
2. Minimize effect of cardiac motion on T2w imaging using saturation band and cardiac gating.
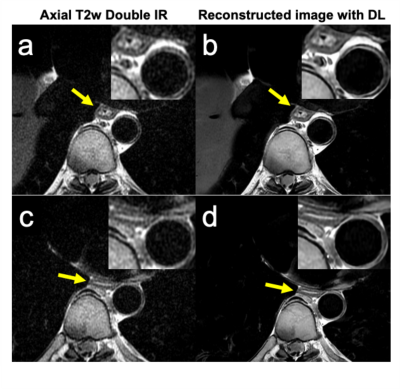
3. Maximize signal to noise ratio (SNR) of T2w images using deep learning (DL) denoising algorithm.
4. Minimize effect of breathing and cardiac motion in DWI using recently proposed, optimized motion-compensated gradient waveforms.
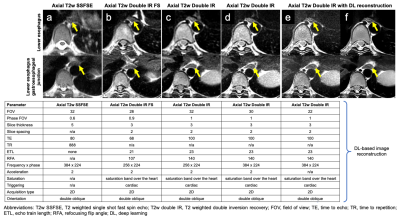
Initially, a standard T2w single shot fast spin echo (SSFSE) sequence was performed in coronal and sagittal view to identify the esophagus, followed by standard axial T2w SSFSE images in double oblique (to long esophageal axis). Next, multiple double oblique T2w double inversion recovery (T2w DIR) images were acquired with different acquisition parameters, such as field of view (FOV) or echo time (TE). For T2w DIR acquisition cardiac gating with saturation band placed over the heart was used. Images were postprocessed using a prototype version of a DL-based image reconstruction pipeline9. All T2w imaging was performed during breath-holding (end-expiration).
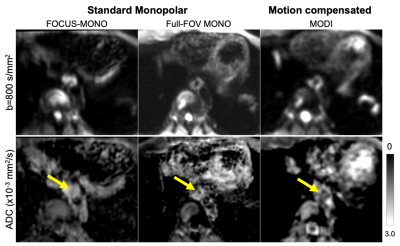
Respiratory-triggered DWI was acquired using three different methods: conventional monopolar (MONO) diffusion encoding waveform with reduced-FOV (50% phase FOV; TE=47-49ms), MONO waveforms with full-FOV (TE= 52.1ms), and an optimized motion-compensated diffusion waveform (to address cardiovascular-related motion artifacts7) with full FOV (TE= 80.4ms) in all patients. Each DWI acquisition was performed in three orthogonal diffusion directions, with b-values (number of averages) of [50(2 repetitions), 800(6 repetitions)]s/mm2. For full-FOV DWI acquisitions: FOV=32cm x 32cm, in-plane resolution=1.25mm x 1.25mm, slice thickness=5mm and parallel imaging factor=2. ADC values were calculated from the averaged DWI images in Matlab (MathWorks, Massachusetts), to be measured by a board-certified radiologist on three esophageal slices using OsiriX Lite software (Pixmeo, Switzerland). Statistical analysis was performed using GraphPad Prism 8.1 (v8.1, GraphPad Software, San Diego). Continuous data are presented as mean ±standard deviation (STD).
Results
Adjustment of T2w DIR sequence parameters including FOV, TE, matrix size and slice thickness, allowed to maximize spatial resolution while maintaining acceptable image quality. An example of the development of a high-resolution T2w protocol can be seen in Figure 1. T2w DIR images with longer TE (100ms), smaller FOV 22mm, and thinner slices (3mm) improved the resolution markedly, compared to standard T2w SSFSE (Figure 1). Further improvement was achieved using cardiac gating and saturation band placed over the heart, which reduced the cardiac-related motion artifacts (Figure 2). Finally, DL reconstruction of the high-resolution T2w images (Figure 3) resulted in low-noise, high-quality T2w image. The mean ADC value of esophageal wall of motion-compensated DWI was 1.632±107 x10-3mm2/s, in comparison to 2.490±387 x10-3mm2/s for reduced-FOV and 2.240±233 x10-3mm2/s and full-FOV MONO (p=0.0108 and p=0.0091, respectively).Discussion
In this work we aimed to improve T2w and DWI MRI of the esophagus. The acquisition protocol improvements in T2w MRI may allow for more accurate assessment of esophageal cancer and add value for diagnostic and therapeutic disease management.The high variability in the measurements (STD) of the standard monopolar diffusion methods (reduced- and full-FOV MONO) indicate substantial bias caused by motion. In contrast, motion-compensated DWI may be less biased and contains less variability, likely due to superior robustness to cardiac-related motion. Further work in larger studies including patients is needed to evaluate the diagnostic accuracy of this novel DWI technique.
Conclusion
This prospective study optimized esophageal MRI by developing high-resolution T2-weighted imaging, with deep learning image reconstruction, and demonstrated feasibility of motion-robust diffusion-weighted imaging (DWI) in vivo.Acknowledgements
This project was supported in part by the Departments of Radiology and Medical Physics, University of Wisconsin. The authors wish to acknowledge support from GE Healthcare and Bracco Diagnostic who provide research support to the University of Wisconsin. Dr. Reeder is a Romnes Faculty Fellow, and has received an award granted by the University of Wisconsin-Madison Office of the Vice Chancellor for Research and Graduate Education with funding from the Wisconsin Alumni Research Foundation.References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians. 2018;68(6):394-424. doi:10.3322/caac.21492
2. Gao Z, Hua B, Ge X, et al. Comparison Between Size and Stage of Preoperative Tumor Defined by Preoperative Magnetic Resonance Imaging and Postoperative Specimens After Radical Resection of Esophageal Cancer. Technol Cancer Res Treat. 2019;18:153303381987626. doi:10.1177/1533033819876263
3. Giganti F, Ambrosi A, Petrone MC, et al. Prospective comparison of MR with diffusion-weighted imaging, endoscopic ultrasound, MDCT and positron emission tomography-CT in the pre-operative staging of oesophageal cancer: results from a pilot study. Br J Radiol. 2016;89(1068):20160087. doi:10.1259/bjr.20160087
4. Heethuis SE, Borggreve AS, Goense L, et al. Quantification of variations in intra-fraction motion of esophageal tumors over the course of neoadjuvant chemoradiotherapy based on cine-MRI. Phys Med Biol. 2018;63(14):145019. doi:10.1088/1361-6560/aacfb5
5. Riddell AM, Allum WH, Thompson JN, Wotherspoon AC, Richardson C, Brown G. The appearances of oesophageal carcinoma demonstrated on high-resolution, T2-weighted MRI, with histopathological correlation. Eur Radiol. 2007;17(2):391-399. doi:10.1007/s00330-006-0363-6
6. Huang YC, Chen TW, Zhang XM, et al. Intravoxel incoherent motion diffusion-weighted imaging of resectable oesophageal squamous cell carcinoma: association with tumour stage. Br J Radiol. 2018;91(1084):20170421. doi:10.1259/bjr.20170421
7. Zhang Y, Peña‐Nogales Ó, Holmes JH, Hernando D. Motion‐robust and blood‐suppressed M 1‐optimized diffusion MR imaging of the liver. Magn Reson Med. 2019;82(1):302-311. doi:10.1002/mrm.27735
8. Peña‐Nogales Ó, Zhang Y, Wang X, et al. Optimized Diffusion‐Weighting Gradient Waveform Design (ODGD) formulation for motion compensation and concomitant gradient nulling. Magn Reson Med. 2019;81(2):989-1003. doi:10.1002/mrm.27462
9. Marc R. L. Performance characterization of a novel deep learning-based MR image reconstruction pipeline. arXiv:2008.06559v1
Figures