0216
Ex vivo quantitative MR characterization of brain lesions induced by SARS-COV-2 infection1Center for NeuroImaging Research - CENIR, Paris Brain Institute - ICM, Paris, France, 2ICM, Sorbonne University, UPMC Univ Paris 06, Inserm U1127, CNRS UMR 7225, Paris, France, 3Hôpital Pitié-Salpêtrière, AP-HP, Paris, France, 4Institut Pasteur, Paris, France
Synopsis
Our study aims to link ex vivo brain MRI signal abnormalities with neuropathological findings relative to the SARS-CoV-2 infection. MRI offers a “big picture” image on the whole organ compared to histology alone, which can be limited to blindly sampled small sections, when recent imagery is not available. The objective is to characterize the brain lesions linked to the viral infection. Our project should produce a new description of the anatomical structures affected by the infection in the central nervous system, and in particular those related to the brain vascular system.
INTRODUCTION
COVID-19 is a major public health problem that has affected almost the entire planet, causing more than 70 million cases and more than 1.6 million deaths (Johns Hopkins University). If most deaths are due to respiratory or cardiovascular failure, it quickly became apparent during the epidemic that the virus had a tropism for the central nervous system (Ellul et al. 2020). The nervous impairment seems to take many forms and its mechanisms, undoubtedly multiple, are being explored. Some signs and symptoms plead for a direct viral attack of the nervous system: anosmia, meningitis and temporal necrotizing encephalitis resembling that of herpes (Moriguchi et al. 2020, Poyiadji et al. 2020). The unusual occurrence of strokes has been noticed in young people (Oxley et al. 2020). Although viral particles have been described in the endothelium of the brain vessels (Paniz-Mondolfi et al. 2020) the presence of the virus within the central nervous system is still debated (Akilesh et al.2020). Neuropathological studies are still few. Relatively few autopsied cases and the lesions observed offer few arguments for direct action by the virus (Solomon et al. 2020). Ante- and post-mortem MRI imaging studies have reported multiple lesions associated with micro-spotting (Coolen et al. 2020). The hypothesis of secondary immune encephalitis has been raised in the face of multiple lesions of the white matter suggestive of ADEM (Reichard et al. 2020). Using postmortem MRI, subcortical micro and macro bleeds were reported (Coolen et al. 2020). Here, we propose a study combining ex vivo imaging by quantitative MRI using R1, R2* and susceptibility mapping (QSM) with a future neuropathological study to elucidate the nature of the lesions observed in COVID patients, their specificity, their pathophysiology whether it is directly linked to viral replication or secondary to the infection.METHODS
The autopsy cases are sampled in accordance with the COVITIS protocol, approved by the national biomedicine agency (Agence de la Biomédecine, PFS 20-008) and the French ministry of research DC2020-4022). Frozen samples are taken from multiple organs to perform a SARS-CoV2 RT-PCR (PATHOCoV study, Sorbonne University). The same regions are sampled to histopathological analysis immediately after brain extraction and cut in the sagittal plane. One hemiencephalon is immersed in 4% formaldehyde while the other one is sampled for cryopreservation. In total, 12 brains were obtained from donors (8 COVID and 4 controls). Ex vivo hemiencephalons obtained from donors were then imaged using a 3T Prisma Fit MRI (Siemens, Germany). A 64-channel head coil was used for signal reception (Siemens, Germany). For imaging, samples were transferred to a vial containing Fluorinert (Sigma, Germany) to decrease the magnetic susceptibility mismatch between the samples and the buffer. MR images were acquired using a 3D Multi Echo Gradient Echo sequence with an isotropic resolution of 500µm. Parameters were: TR = 42 ms, TEs ranging from 3 to 38 ms with a ΔTE of 5 ms (8 echoes acquired). Flip angle was 30° and number of averages was 4 leading to a scan time of 2.5 hours. This protocol was repeated with a second acquisition where we just modified the flip angle (10°) for further R1 mapping. B1 mapping was also performed. Total scan time was around 5 hours per brain. Images of multiple echoes were combined using a root mean square, thus providing both high SNR and T2*-contrasted images. Longitudinal relaxation rate (R1) was obtained using the variable flip angle technique and B1 correction using the qMRLab built-in functions. Transversal relaxation rate (R2*) was evaluated using a nonlinear fitting method in Matlab (Mathworks, USA). Quantitative Susceptibility Mapping (QSM) images were reconstructed using MEDI Toolbox for both background field filtering and dipole inversion, using respectively Laplacian Boundary Value (LBV) and L1-MEDI functions.RESULTS
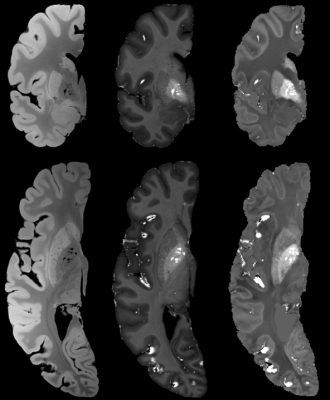
We obtained preliminary results on the first 3 COVID brains. The presented protocol allowed to obtain high resolution quantitative maps for R1, R2* and QSM. We found numerous dark spots on T2*-weighted images in the Globus Pallidus in two different brains that were identified as microhemorrhages using both R2* and QSM values, see figure 1. R1 mapping did not show any abnormal values on any brains. No other lesions were detected using this approach.DISCUSSION AND CONCLUSION
Due to difficulties induced by the successive confinements, the completion the study was delayed. Especially, only one fourth of the cohort data was acquired and neuropathological study is still ongoing. However, among preliminary results, multiple microhemorrhages were observed in one patient, who has been investigated with both histopathological and virological methods. We intend to complete data collection, as well as combining to other MR metrics such ex vivo diffusion MRI to infer any modifications on brain structural connectivity.Acknowledgements
This work was supported by a joint internal
grant of Paris Brain Institute and Institut Pasteur.
References
Akilesh S. et al Characterizing Viral Infection by Electron Microscopy Lessons from the Coronavirus Disease 2019 Pandemic, The American Journal of pathology, In press.
Cabana J.-F. et al. (2016) Quantitative magnetization transfer imaging made easy with qMTLab: Software for data simulation, analysis, and visualization. Concepts Magn. Reson
Coolen, T et al. (2020) Early postmortem brain MRI findings in COVID-19 non-survivors. Neurology.
Ellul, M. A., et al. (2020) Neurological associations of COVID-19. Lancet Neurol.
Liu J et al. Neuroimage 2011.
Moriguchi, T. et al. (2020) A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis, 94, 55-58.
Oxley, T. J., et al. (2020) Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N Engl J Med, 382, e60.
Paniz-Mondolfi, A., et al. (2020) Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol, 92, 699-702.
Poyiadji, N., et al. (2020) COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: CT and MRI Features. Radiology, 201187.
Reichard, R. R., et al. (2020) Neuropathology of COVID-19: a spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology. Acta Neuropathol, 140, 1-6.
Zhou D et al. NMR Biomed. 2014 Mar; 27(3).
Figures