0215
Evaluation for Myocarditis in Competitive Athletes Recovering from COVID-19 using Cardiac MRI1Radiology, University of Wisconsin-Madison, Madison, WI, United States, 2Medicine, University of Wisconsin-Madison, Madison, WI, United States, 3Biomedical Engineering, University of Wisconsin-Madison, Madison, WI, United States, 4Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 5Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States
Synopsis
Recent reports of COVID-19-associated myocarditis have raised safety concerns for athletes returning to training after recovering from COVID-19. As a result, our institution initiated a comprehensive screening program for all student athletes recovering from COVID-19, to screen for myocarditis using non-invasive diagnostic tests, including cardiac MRI. In this retrospective study we describe our institutional experience, including the prevalence and severity of MRI findings of myocarditis in student athletes recovering from COVID-19. Patients had mild (73/149;49%) or moderate symptoms (40/149;27%), or were asymptomatic (26/149;17%). Only 2/149 patients had MRI findings consistent with updated Lake Louise criteria for myocarditis (1.3%, 95%CI 0.4%,4.8%).
Introduction
After outbreaks of the novel coronavirus disease 2019 (COVID-19) in late 2019, and in early 2020 in the United States, many complications of this disease have been reported, including report describing COVID-19-asscociated myocarditis based on cardiac MRI findings1.Myocarditis is an inflammatory condition associated with viral disease with heterogeneous clinical presentation and a course ranging from asymptomatic to fulminant2,3. Contrast-enhanced cardiac MRI is a well-established technique for the detection of myocarditis4. Myocarditis is associated with sudden cardiac death in young athletes5. In a recent case series from the Ohio State University, 15% (4/26) of athletes recovering from COVID-19 were found to have findings consistent with myocarditis on cardiac MRI1. The clinical significance of these findings and outcomes for reported athletes remains unknown at this time.
Given recent reports of COVID-19-associated myocarditis in athletes, and with growing numbers of COVID-19 cases on campus, our institution has initiated a screening program to evaluate all student athletes testing positive for COVID-19, using noninvasive diagnostic methods, including cardiac MRI. Thus, the purpose of this work is to describe the prevalence as well as severity of cardiac MRI findings of myocarditis in competitive student athletes recovering from COVID-19.
Methods
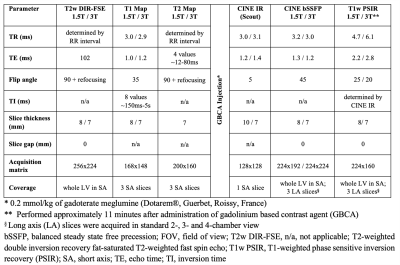
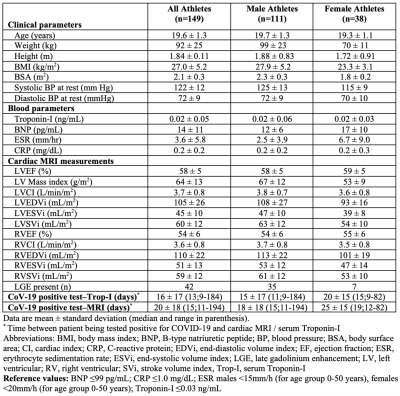
This retrospective study was performed with Institution Review Board approval, including a waiver of informed consent and a waiver of HIPAA authorization. In this study, a search in the electronic health records was performed to identify all competitive student athletes recovering from COVID-19, who underwent contrast-enhanced cardiac MRI between January 1st and December 12th, 2020. MRI findings were validated by two radiologists experienced in cardiac imaging, using updated Lake Louise criteria. Further, relevant clinical data, electrocardiogram (ECG) and transthoracic echocardiography (TTE) findings, as well as serum markers including troponin-I, B-type natriuretic peptide, C-reactive protein, erythrocyte sedimentation rate were recorded.A standardized cardiac MRI protocol was performed in all athletes, in accordance with guidelines by the Society for Cardiac Magnetic Resonance6. This included (Table 1): CINE imaging in short axis (SA) and three standardized long axis (LA) planes (in 2-, 3- and 4-chamber view); double inversion recovery fat-saturated T2-weighted imaging for evaluation of myocardial edema in SA; native T1- and T2-mapping in SA; and late gadolinium enhancement (LGE) imaging in SA and LA. Imaging was performed on clinical 1.5T or 3T MRI systems (GE Healthcare) and analyzed using cvi42® software (Circle Cardiovascular Imaging, Calgary, Alberta, Canada).
ECGs performed for each athlete were compared to baseline ECG, which was obtained as part of pre-participation evaluation. Date of onset, type and severity of COVID-19 symptoms (if any) and date of positive reverse transcriptase polymerase chain reaction (rt-PCR) test were recorded.
Results
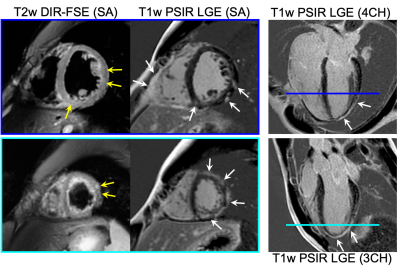
149 competitive athletes (111 male/38 female, mean age 20 years, range 17-23 years) recovering from COVID-19 were identified (Table 2), who underwent cardiac MRI at 1.5T (79/149) and 3T (70/149). Cardiac MRI was performed 20 ±18 days (median 15 days; range 11-194). A diagnosis of COVID-19 using rt-PCR was confirmed in all patients.Myocarditis was detected on cardiac MRI in 2/149 patients (1.3%, 95%CI, 0.4%, 4.8%). One of these two patients had marked MRI findings of myopericarditis (myocardial edema and LGE over multiple segments, pericardial enhancement; Figure 1). This patient was initially asymptomatic and tested positive for COVID-19 during routine screening. Troponin-I in this patient was normal prior to MRI, however, it became pathologically increased two days after MRI (0.04 ng/mL), peaking at 0.09 ng/mL (normal ≤0.03 ng/mL) four days later. ECG detected nonspecific ST-T wave abnormalities. TEE revealed nonspecific mild reduction in global left ventricular longitudinal strain. The clinical follow-up one month after MRI revealed one episode of mild dyspnea.
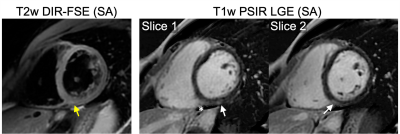
The second patient had mild MRI findings of myocardial inflammation with mild myocardial edema and 1cm LGE at the inferior basal LV wall (Figure 2). The patient had mild viral infection symptoms for couple of days. TTE, ECG and serum markers were normal in this patient.
A small nonspecific focal enhancement in the septum at the right ventricular insertion was observed in 38/149 (26%) patients. Lake Louise MRI criteria for myocarditis were not met in these patients. This MRI finding was interpreted to be related to athletic training.
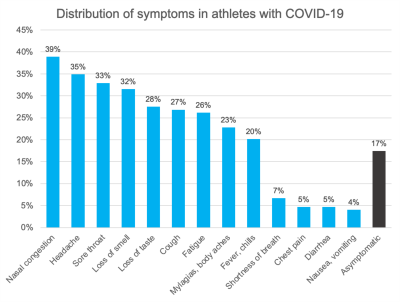
Most of the patients were symptomatic 120/149 (81%) with mild (73/149;49%) and moderate (40/149;27%) symptoms. Symptoms were not specified in 7/149 (5%) patients, and not documented in 3/149 (2%) patients. 26/149 (17%) patients were asymptomatic. The most common symptoms (Figure 3) included congestion (58/149;39%), headache (52/149;35%) and sore throat (49/149;33%). No patient experienced severe symptoms requiring hospitalization or received antiviral drugs. The majority of ECGs and TTEs were negative or had minor, nonspecific abnormalities not indicative of myocarditis.
Discussion
This study was a comprehensive evaluation of competitive student athletes recovering from COVID-19 evaluated at our institution. Our results demonstrated a low prevalence of myocarditis among asymptomatic and mild-to-moderately symptomatic student athletes based on cardiac MRI and ancillary tests.Conclusion
Based on our findings, we conclude that the use of cardiac MRI to screen competitive athletes who are asymptomatic or mild-to-moderately symptomatic and have normal ancillary tests is questionable. Further studies are needed to confirm this conclusion.Acknowledgements
The authors acknowledge GE Healthcare and Bracco Diagnostics who provide research support to the University of Wisconsin-Madison. L.L.E. is funded in part by the Gary and Marie Weiner Professorship in Cardiovascular Medicine Research. S.B.R. is a Romnes Faculty Fellow, and has received an award provided by the University of Wisconsin-Madison Office of the Vice Chancellor for Research and Graduate Education with funding from the Wisconsin Alumni Research Foundation.References
1. Rajpal S, Tong MS, Borchers J, et al. Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering From COVID-19 Infection. JAMA Cardiol. Published online September 11, 2020. doi:10.1001/jamacardio.2020.4916
2. Andréoletti L, Lévêque N, Boulagnon C, Brasselet C, Fornes P. Viral causes of human myocarditis. Archives of Cardiovascular Diseases. 2009;102(6-7):559-568. doi:10.1016/j.acvd.2009.04.010
3. Tschöpe C, Ammirati E, Bozkurt B, et al. Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat Rev Cardiol. Published online October 12, 2020. doi:10.1038/s41569-020-00435-x
4. Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation. Journal of the American College of Cardiology. 2018;72(24):3158-3176. doi:10.1016/j.jacc.2018.09.072
5. Maron BJ, Haas TS, Ahluwalia A, Murphy CJ, Garberich RF. Demographics and Epidemiology of Sudden Deaths in Young Competitive Athletes: From the United States National Registry. The American Journal of Medicine. 2016;129(11):1170-1177. doi:10.1016/j.amjmed.2016.02.031
6. Schulz-Menger J, Bluemke DA, Bremerich J, et al. Standardized image interpretation and post-processing in cardiovascular magnetic resonance - 2020 update: Society for Cardiovascular Magnetic Resonance (SCMR): Board of Trustees Task Force on Standardized Post-Processing. J Cardiovasc Magn Reson. 2020;22(1):19. doi:10.1186/s12968-020-00610-6
Figures