0189
Preliminary study on free respiratory navigation whole-heart coronary magnetic resonance angiography based on Dixon at 3.0 T1The First Affiliated Hospital of Dalian Medical University, Dalian, China, Dalian, China
Synopsis
In comparison with the traditional whole-heart coronary magnetic resonance angiography (WH-CMRA) based on the spectral pre-saturation with inversion recovery (SPIR), the advanced WH-CMRA based on Dixon with non-contrast-enhanced free respiratory navigation is associated with advantages of improved image quality, increased blood signal-to-noise ratio, and the extra fat image. This study proved that it is feasible to visualize the coronary artery (image quality scores met the requirement of clinical diagnosis) using the Dixon based WH-CMRA without increasing scan time.
Main findings
This study proved that it is feasible to visualize the coronary artery using the Dixon based whole-heart coronary magnetic resonance angiography.Introduction
Previous studies have shown that, in comparison with the traditional spectral pre-saturation with inversion recovery (SPIR), the whole-heart coronary magnetic resonance angiography (WH-CMRA) based on the Dixon sequence can provide improved image quality, increased blood signal-to-noise ratio at 1.5 T [1] and 3 T [2], and an extra fat image with more diagnostic information [3-4]. This study aims to explore the feasibility of the Dixon-based WH-CMRA for coronary artery visualization in patients with chest discomfort but no exact history of coronary heart disease.Materials and methods
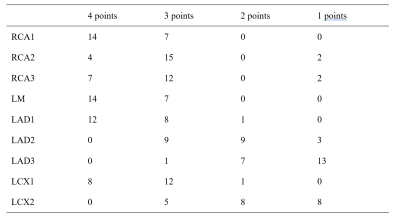
This study has been approved by the local IRB. 21 patients (12 males, age 44-82 years) were recruited and underwent the WH-CMRA scan on a 3.0 T MR scanner (Ingenia CX, Philips Healthcare, Best, the Netherlands) with free breathing diaphragm navigation. Before scan of the Dixon sequence, the phase imaging was repeatedly performed by 100 times to observe the movement track of the right coronary artery on the axial image, and thus to modified the individualized setting of trigger delay (TD) and the relatively stationary duration. Scanning parameters of Dixon included: TR/TE = 4/0 ms, flip angle = 10°, FOV = 301×301 mm2, matrix size = 200×201, spatial resolution = 1.5×1.7 mm2, slice thickness = 1.5 mm, and slice gap = 0.8 mm. Standard cardiac volume shim was used, and the size of gating window was 4 mm.All images were reconstructed using the platform of Intelli Space Portal (Philips Healthcare). Coronary arteries were divided into 4 branches [5] including right coronary artery (RCA), left main coronary artery (LM), left anterior descending artery (LAD) and left coronary circumflex artery (LCX). The 4 branches were further divided into 9 segments including the RCA proximal, mid and distal segments (RCA1, RCA2, RCA3), LAD proximal, mid and distal segments (LAD1, LAD2, LAD3), LCX proximal and distal segments (LCX1, LCX2), and the LM segment. Two radiologists scored the image quality with the following criteria: 1 points: coronary artery is severely obscure or barely visible; 2 points: coronary artery can be observed with moderately obscure boundary; 3 points: coronary artery can be observed with slightly obscure boundary; 4 points: coronary arteries can be observed with clear vascular boundary (Figure 1).
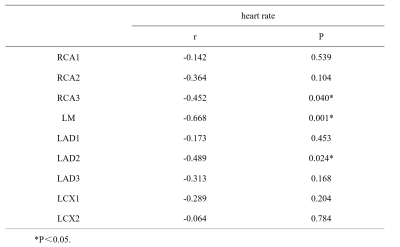
Kappa test was used for consistency of image quality scores by given by the two observers. Spearman correlation analysis was used to observe the correlation between coronary artery image quality score and heart rate of each segment. P < 0.05 was considered statistically significant.
Results
The average scan time of 21 subjects was 5.21±0.96min, resulting in a total of 84 coronary arteries and 189 segments. Image quality scores given by the observers were in good agreement (Kappa=0.753). The number of coronary segments with image quality scores of 4, 3, 2 and 1 were 59 (31.22%), 76 (40.21%), 30 (15.87%), and 24 (12.70%), respectively (Table 1). A total of 165 (87.30%) coronary segments met the diagnostic requirements (≥2 points).Heart rate showed significant negative correlations to the image quality scores for RCA3, LM, and LAD2 (r=-0.452,P=0.040;r=-0.668,P=0.001;and r=-0489,P=0.024, respectively) rather than to those of other segments (Table 2).
Conclusion
The Dixon sequence does not increase the scan time in comparison with PSIR. Results indicated that most of the measurements by the Dixon based WH-CMRA met the requirements of clinical diagnosis. Therefore, it is feasible to visualize coronary artery using the non-contrast-enhanced free respiratory navigation Dixon-based WH-CMRA. Significant correlations of the heart rate to the image quality scores indicate that visualizations of the right coronary artery and the left proximal coronary artery are associated with better stability.Acknowledgements
No acknowledgementReferences
[1] Börnert P, Koken P, Nehrke K, et al. Water/fat-resolved whole-heart Dixon coronary MRA: an initial comparison. Magn Reson Med. 2014;71:156-163.
[2] Nezafat M, Henningsson M, Ripley DP et al. Coronary MR angiography at 3T: fat suppression versus water-fat separation.MAGMA. 2016;29:733-738.
[3] Ma J, Dixon techniques for water and fat imaging. J Magn Reson Imaging. 2008;28:543-558.
[4] Kellman P, Hernando D, Shah S, et al. Multiecho dixon fat and water separation method for detecting fibrofatty infiltration in the myocardium. Magn Reson Med. 2009;61:215-221.
[5] Austen WG, Edwards JE, Frye RL et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975;51:5-40.
Figures