0185
Assessing the Prognosis of Acute Deep Vein Thrombosis Using Magnetic Resonance Black-blood Thrombus Imaging1Department of Biomedical Engineering, Guangzhou Medical University, Guangzhou, China, 2Department of Radiology, Guangzhou Panyu Central Hospital, Guangzhou, China, 3Department of Minimally Invasive Interventional Radiology, Guangzhou Panyu Central Hospital, Guangzhou, China, 4Department of Anesthesiology, Mindong Hospital, Ningde, China, 5MR Collaborations, Siemens Healthcare Ltd, Shenzhen, China, 6Philips Healthcare, Guangzhou, China, 7Biomedical Imaging Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA, United States, 8Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, United States
Synopsis
Patients with acute deep vein thrombosis (DVT) can be characterized as iso- or hyper-intense thrombus signals using a T1-weighted black-blood magnetic resonance imaging (BTI) technique. Patients with hyper-intense thrombus signals demonstrated a significant higher incidence of post-thrombotic syndrome (PTS) than those with iso-intense thrombus signals, regardless of the patient’s age, gender, the severity of DVT, and the treatment strategy of catheter-directed thrombolysis or conventional anticoagulant therapy. The results suggest that the thrombus signal characteristics obtained on BTI imaging are valuable for assessing the prognosis of acute DVT and may aid in guiding the clinical treatment plan.
Background
DVT occurs when blood clots form in one or more leg veins, which may precede a potentially fatal pulmonary embolism and can also lead to PTS1. Previous animal study demonstrated that MR can be used to evaluate the lysis of deep vein thrombosis2. However, the evaluation has not been reported for humans in a clinical cohort. This study aimed to evaluate the imaging and clinical outcomes of lysis in acute DVT patients using thrombus signal characteristics generated by BTI.Methods
Acute DVT patients (≤14 days of symptom onset) were consecutively enrolled and given BTI scans. Scan parameters were the same as previous studies3. The patients were randomly assigned to catheter-directed thrombolysis (CDT) or conventional anticoagulant therapy. The patients from each group were further divided into iso- or hyper-intense thrombus subgroups based on the thrombus signal characteristics of BTI images. The patients treated with CDT were assessed by thrombolysis ratio according to the method of Porter and Moneta4. PTS was diagnosed for all patients using the Villalta score5. Primary outcomes were evaluated by clinical visits at 1, 6, and 12 months after treatment. Statistical analyses were performed to compare primary outcomes between patients with iso- and hyper-intense thrombus. Histology and iron quantification were performed to characterize the composition of the iso- or hyper- intense thrombus.Results
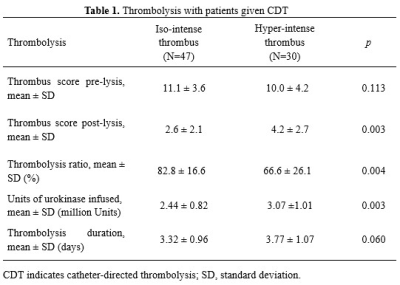
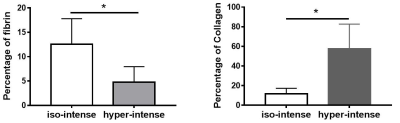
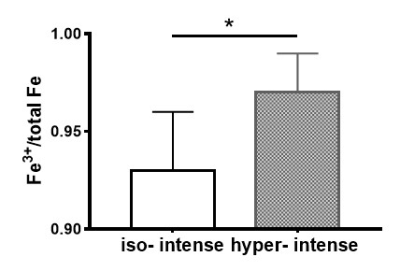
168 patients were included in the per-protocol analysis, including 77 patients undergoing CDT and 91 patients undergoing anticoagulation. Venous thrombosis was identified on BTI images of all patients. Based on the thrombus signal contrast, 47 out of 77 (61%) patients receiving CDT and 49 out of 91 (54%) patients receiving conventional anticoagulation presented with iso-intense thrombus, while the remaining patients presented with hyper-intense thrombus. Representative images of patients with iso- and hyper-intense thrombus are shown in Figure 1. The duration of symptoms of the patients with iso-intense thrombus was significantly shorter than that of the patients with hyper-intense thrombus (CDT group:6.1±3.5 days vs. 9.9±4.5, p<0.001; anticoagulation group: 5.5±3.2 days vs. 8.8±4.0, p<0.001). Patients treated with CDT had significantly higher thrombolysis ratio in iso-intense thrombus subgroup than in the hyper-intense thrombus subgroup (Table 1). For both CDT and conventional anticoagulant subgroups, there was no significant difference in PTS incidence between patients with iso- and hyper-intense thrombus at 1-month follow-up. However, patients with iso-intense thrombus had significantly lower incidence rates of PTS than those with hyper-intense thrombus at 6 and 12 months (Table 2). Iron quantification and histology demonstrated that iso-intense thrombus had higher content of fibrin and a lower ratio of Fe3+ to total iron than hyper-intense thrombus (Figure 2&3).Discussion
The signal contrast of thrombus relative to the surrounding muscle on BTI images was found to successfully predict the outcome of treatment in DVT patients. Patients with iso-intense thrombus had better treatment results and lower PTS incidence than those with hyper-intense when treated with CDT or conventional anticoagulation.It has been reported that iron, gradually brought into the thrombus by fibrin-trapped red blood cells, is oxidized through inducible nitric oxide synthase. This results in the accumulation of paramagnetic Fe3+ that can shorten the T1 relaxation time of the thrombus6. Thus, the T1 relaxation time of the thrombus in the acute phase gradually becomes shorter, and the thrombus appears brighter on T1-weighted MR images. This was confirmed by the iron quantification results: the ratio of Fe3+ to total iron is higher in hyper- than iso-intense thrombus (Figure 3). Furthermore, the study demonstrates that the average duration of symptoms in the patients with iso-intense thrombus signals was significantly shorter than that of the patients with hyper-intense signals. This evidence suggests that acute thrombus with iso-intense signals is in an earlier stage than thrombus with hyper-intense signal.
A previous study has shown that the effect of lytic therapy on a thrombus can be predicted by the thrombus T1 relaxation time: a short T1 relaxation time <747 ms (i.e., hyper intensity signal) was a good predictor of DVT lysability in a murine model study2. However, this was in a conflict with our findings that the lysability is associated with an isointense (i.e., long T1 relaxation time) thrombus in acute phase. Higher content of fibrin was observed in the murine thrombus with short T1 relaxation time (i.e., HIT) by Saha et al2. In contrast, this study has demonstrated a higher content of fibrin in the human thrombus with iso-intense signal (Figure 2). Since the target of urokinase and other thrombolytic drugs is fibrin, it follows that the lysis effect may be more pronounced for iso-intense human thrombus. The conflict between our study and Saha et al might be due to differences between human and mice, which could involve in different thrombotic components, drug resistance, and autolysis systems.
Conclusions
Thrombus signal characteristics on BTI are valuable to infer the incidence of PTS in acute DVT patients treated with either additional CDT or conventional anticoagulation.Acknowledgements
This work was supported in part by the National Science Foundation of China (81971607, 81729003), and the Guangzhou Science and Technology Project (201804010240).References
1. Heit JA. The epidemiology of venous thromboembolism in the community. Arterioscler Thromb Vasc Biol. 2008;28:370-372.
2. Saha P, Andia ME, Modarai B, Blume U, Humphries J, Patel AS, Phinikaridou A, Evans CE, Mattock K, Grover SP, et al. Magnetic resonance t1 relaxation time of venous thrombus is determined by iron processing and predicts susceptibility to lysis. Circulation. 2013;128:729-736.
3. Chen H, He X, Xie G, Liang J, Ye Y, Deng W, He Z, Liu D, Li D, Liu X, et al. Cardiovascular magnetic resonance black-blood thrombus imaging for the diagnosis of acute deep vein thrombosis at 1.5 tesla. J Cardiovasc Magn Reson. 2018;20:42.
4. Porter JM, Moneta GL. Reporting standards in venous disease: An update. International consensus committee on chronic venous disease. Journal of vascular surgery. 1995;21:635-645.
5. Kahn SR, Partsch H, Vedantham S, Prandoni P, Kearon C, on behalf of the Subcommittee on Control of Anticoagulation of the S, Standardization Committee of the International Society on T, Haemostasis. Definition of post-thrombotic syndrome of the leg for use in clinical investigations: A recommendation for standardization. Journal of thrombosis and haemostasis : JTH. 2009;7:879-883.
6. Nishimoto Y, Yamashita Y, Morimoto T, Saga S, Amano H, Takase T, Hiramori S, Kim K, Oi M, Akao M, et al. Risk factors for post-thrombotic syndrome in patients with deep vein thrombosis: From the command vte registry. Heart Vessels. 2019;34:669-677.
Figures