0140
Quantitative DCE and DW-MRI to Evaluate Suspicious Mammographic Calcifications: Results from a Single Institution Prospective Clinical Trial
Janis M. Yee1, Daniel S. Hippe1, Michael Hirano1, Bonny Chau1, Debosmita Biswas1, Anum S. Kazerouni1, Mary Lynn Bryant1, Isabella Li1, Jennifer Xiao1, Wei Huang2, Savannah C. Partridge1, and Habib Rahbar1
1Radiology, University of Washington, Seattle, WA, United States, 2Oregon Health & Science University, Portland, OR, United States
1Radiology, University of Washington, Seattle, WA, United States, 2Oregon Health & Science University, Portland, OR, United States
Synopsis
Mammographic calcifications remain a diagnostic dilemma with low positive predictive value for malignancy. Our study investigated the use of quantitative DCE and DW-MRI metrics to problem solve suspicious calcifications prior to biopsy. In patients with a suspicious enhancing MRI correlate, malignant lesions exhibited higher peak PE, peak SER, functional tumor volume, and Ktrans. Basic and advanced 3D DW-MRI parameters did not yield statistically significant discriminatory values in this small pilot study. Use of quantitative MRI features shows potential to reduce the number of unnecessary biopsies for suspicious mammographic calcifications among the subset that demonstrate suspicious enhancement.
Introduction
Mammographic calcifications are associated with nearly half of clinically occult breast cancers, with the majority linked to ductal carcinoma in situ (DCIS).1 However, the positive predictive value (PPV) for malignancy of pure calcifications remains low, ranging from 15-40%.2 Breast MRI has been proposed as a means to problem solve mammographically-detected calcifications due to its high sensitivity (reported as high as 94-100%).3 However, specificity and PPV for malignancy on the basis of clinical features alone is modest; thus, the use of conventional MRI alone still results in many unnecessary biopsies. Prior studies have shown that quantitative lesion analysis using a combined high spatial and high temporal resolution acquisition can provide discriminatory value to differentiate benign from malignant lesions. Furthermore, advanced diffusion weighted imaging metrics, including intravoxel incoherent motion (IVIM)-derived parameters, hold promise to provide complementary MRI signatures to further improve the characterization of breast lesions.4-6 The purpose of our study was to investigate if these quantitative MRI parameters could be used to accurately predict benign or malignant pathology of suspicious mammographic calcifications presenting as suspicious enhancement on MRI.Materials and Methods
This IRB-approved, HIPAA-compliant, prospective study (Clinical Trials.org NCT03495011) included 76 women with 79 unique areas of previously identified mammographic calcifications who provided informed consent prior to undergoing a research 3T dynamic contrast-enhanced (DCE) and multi-b value (0, 10, 20, 30, 50, 70, 100, 150, 200, 400, 600, 800, 1000 s/mm2) diffusion weighted MRI (DW-MRI) from April 2018 to March 2020. All MRIs were performed prior to biopsy of the calcifications. DCE-MRI was performed using a hybrid acquisition combining high temporal resolution keyhole-based (variable 6.9-30s sampling, 23 total acquisitions) and high spatial resolution (0.8 × 0.8 mm2, three total acquisitions, pre-contrast, 2 and 7 min post-contrast) techniques. MRIs were prospectively interpreted by a fellowship-trained breast imaging radiologist prior to biopsy, referencing the mammographic findings. Calcifications with an enhancing correlate underwent quantitative 3D lesion MRI analysis. DCE-MRI data was fit to the Kety-Tofts model to extract pharmacokinetic parameters (Ktrans, ve, kep). Additional features including signal enhancement ratio (SER), percent enhancement (PE), functional tumor volume (FTV), and washout fraction were obtained. Peak PE and peak SER were determined for hot-spot regions producing the highest PE and SER values. DW-MRI data was analyzed to extract apparent diffusion coefficient (ADC), pseudodiffusion (Dp), true diffusion coefficient (Dt), and perfusion fraction (f) for each lesion (Figure 1). Reference standard for all lesions was histopathological evaluation of core needle biopsies (CNB) obtained via stereotactic biopsy and surgical excision for malignant lesions. The ability of each quantitative MRI parameter to discriminate benign and malignant lesions was summarized using the area under the receiver operating characteristic curve (AUC) and tested using the Wilcoxon rank-sum test.Results
Of the entire cohort of 79 calcifications, 22 were malignant (9 high grade DCIS, 6 non-high grade DCIS, 7 invasive carcinoma) resulting in a PPV of 28% (22/79) on mammography alone. Twenty-three out of 79 calcifications demonstrated a suspicious enhancing correlate on MRI, of which 15 were malignant (6 high grade DCIS, 3 non-high grade DCIS, 6 invasive carcinoma) for a PPV of 65% (15/23) and a negative predictive value of 88% (49/56; 3 high grade DCIS, 3 non-high grade DCIS, and 1 invasive carcinoma demonstrated no suspicious enhancement). Included women were mean age 56 ±10 years; 70% (16/23) had mammographically dense breasts while 65% (15/23) had minimal/mild background parenchymal enhancement on MRI (Table 1). Malignant lesions exhibiting suspicious enhancement demonstrated higher peak PE (mean: 209 ±45 vs. 158 ±48, AUC=0.82, p=0.013), peak SER (mean: 1.22 ±0.23 vs. 1.06 ±0.19, AUC=0.77, p=0.040), FTV (median: 1.34 cm3 vs. 0.23 cm3, AUC=0.93, p<0.001), and Ktrans (mean: 0.06 ±0.03 s-1 vs. 0.05 ±0.02 s-1, AUC=0.76, p=0.047) than benign lesions (Table 2). Washout fraction, ve, and kep were not statistically significantly different between malignant and benign lesions (p>0.05). Of the 23 suspicious enhancing lesions, 19 (13 malignant, 6 benign) demonstrated a DW-MRI correlate free from significant artifact that allowed for quantitation. No basic or advanced diffusion parameters were found to provide discrimination between benign and malignant lesions, although f (mean: 0.09 ±0.03 vs. 0.17 ±0.12, AUC=0.71, p=0.18) showed potential value (Table 2).Conclusion and Discussion
Results from this prospective trial show that specific quantitative measures of enhancing MRI correlates to mammographically suspicious calcifications can assist with differentiating benign from malignant pathologies and thereby further decrease unnecessary biopsies. These findings are consistent with prior reports on the use of quantitative DCE parameters 7, 8 to discriminate among benign and malignant lesions. Although no DW-MRI feature added significant value in this small study, IVIM perfusion fraction showed a potential trend that could be studied in larger cohorts. Additional studies are warranted to further investigate advanced DW-MRI parameters and their utility to problem solve suspicious calcifications as well as serve as prognostic markers for the subset of DCIS lesions that represent possible overdiagnosis.Acknowledgements
This study was supported by NIH/NCI grants R01CA203883, R01CA207290 and R01CA248192.References
- Stomper PC, Geradts J, Edge SB, Levine EG. Mammographic predictors of the presence and size of invasive carcinomas associated with malignant microcalcification lesions without a mass. AJR Am J Roentgenol. Dec 2003;181(6):1679-84. doi:10.2214/ajr.181.6.1811679
- Shehata M, Grimm L, Ballantyne N, et al. Ductal Carcinoma in Situ: Current Concepts in Biology, Imaging, and Treatment. Journal of Breast Imaging. 2019;1(3):166-176. doi:10.1093/jbi/wbz039
- Liberman L, Morris EA, Lee MJ-Y, et al. Breast Lesions Detected on MR Imaging: Features and Positive Predictive Value. American Journal of Roentgenology. 2002/07/01 2002;179(1):171-178. doi:10.2214/ajr.179.1.1790171
- Tao WJ, Zhang HX, Zhang LM, et al. Combined application of pharamcokinetic DCE-MRI and IVIM-DWI could improve detection efficiency in early diagnosis of ductal carcinoma in situ. J Appl Clin Med Phys. Jul 2019;20(7):142-150. doi:10.1002/acm2.126245.
- Partridge SC, Nissan N, Rahbar H, Kitsch AE, Sigmund EE. Diffusion-weighted breast MRI: Clinical applications and emerging techniques. https://doi.org/10.1002/jmri.25479. Journal of Magnetic Resonance Imaging. 2017/02/01 2017;45(2):337-355. doi:https://doi.org/10.1002/jmri.25479
- Liu C, Liang C, Liu Z, Zhang S, Huang B. Intravoxel incoherent motion (IVIM) in evaluation of breast lesions: Comparison with conventional DWI. European Journal of Radiology. 2013;82(12):e782-e789. doi:10.1016/j.ejrad.2013.08.006
- Arasu VA, Chen RCY, Newitt DN, et al. Can signal enhancement ratio (SER) reduce the number of recommended biopsies without affecting cancer yield in occult MRI-detected lesions? Academic radiology. 2011;18(6):716-721. doi:10.1016/j.acra.2011.02.008
- Jansen SA, Fan X, Karczmar GS, Abe H, Schmidt RA, Newstead GM. Differentiation between benign and malignant breast lesions detected by bilateral dynamic contrast-enhanced MRI: a sensitivity and specificity study. Magnetic resonance in medicine. 2008;59(4):747-754. doi:10.1002/mrm.21530
Figures
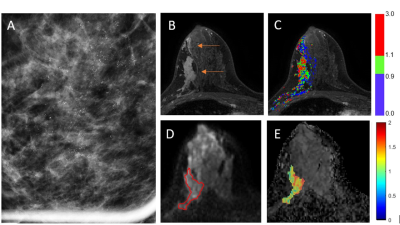
Figure 1. 45-year-old
woman with ILC presenting with screen-detected mammographic calcifications. (A) Magnification view shows fine pleomorphic
calcifications. (B) DCE-MRI prior to biopsy demonstrates suspicious segmental NME (arrows) at the site of the
calcifications. (C) SER map shows mixed kinetic features and washout
(SER > 1.1, red) in the dominant part of the lesion. (D) DW-MRI (b=800
s/mm2) demonstrates slightly hyperintense signal in this area (red outline = segmented lesion) relative to normal tissue.
(E) ADC map shows mean ADC = 1.27 x 10-3 mm2/s for the lesion (in color).

Table 1: Patient and lesion characteristics
for the 23 included women with mammographic calcifications demonstrating a
suspicious enhancing MRI correlate.
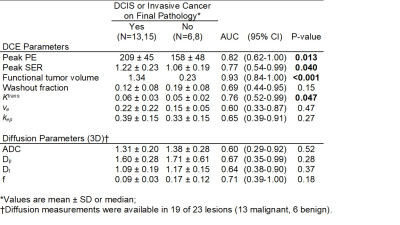
Table 2: Comparison of individual
quantitative DCE and DW-MRI parameters between benign and malignant lesions.