0014
The power of field strength: a direct comparison of USPIO-enhanced MRI at 3 and 7T to detect suspicious lymph nodes in patients with prostate cancer1Radboudumc, Nijmegen, Netherlands, 2Radiology, Ziekenhuis Gelderse Vallei, Ede, Netherlands, 3Erwin L Hahn Institute for MR Imaging, Essen, Germany, 4University of Heidelberg, Heidelberg, Germany, 5University of Duisburg-Essen, Essen, Germany
Synopsis
Lymph node metastases in prostate cancer patients are mainly found in normal sized lymph nodes and detection is a major challenge. USPIO-enhanced MRI with ferumoxtran-10 discriminates between normal and suspicious lymph nodes. We examined 20 prostate cancer patients with high risk of advanced disease with USPIO-enhanced MRI at 3 and at 7 Tesla, and compared the amount, the level of suspicion, and the size of lymph nodes with two readers. More, but on average not larger suspicious nodes were annotated on 7T versus 3T MRI by both readers, with less interobserver variability at 7T.
Introduction
The detection of lymph node metastases in prostate cancer is a continuous challenge. An extended pelvic lymph node dissection is the gold standard for lymph node staging in patients with prostate cancer, but clinical outcome does not differ between high or intermediate risk prostate cancer in whom pelvic lymph node dissection was or was not performed at radical prostatectomy1,2. Reasons could be that lymph node metastases are often small3,4 and therefore missed with dissections, or that a substantial number of nodal metastases is located outside the resection field5. Ferumoxtran-10 enhanced MRI for lymph node detection does not depend on size or location of affected lymph nodes. This ultrasmall super paramagnetic iron oxide (USPIO) particle accumulates in normal lymph nodes attenuating their signal on T2*-weighted images. Lymph nodes that retain MR signal do not accumulate USPIO particles and are suspicious for metastasis. Earlier research showed improved image quality of USPIO-enhanced MRI on 3T MRI compared to 1.5T6. At an ultra-high field strength of 7T spatial resolution may be further improved and therefore more and possibly smaller lymph nodes may be detected7. In this study we compared the detection of suspicious lymph nodes in prostate cancer patients on 7T MRI compared to 3T MRI.Materials and Methods
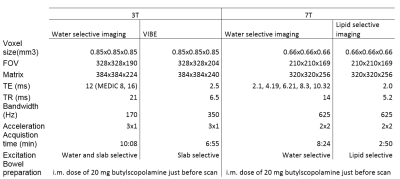
Twenty consecutive prostate cancer patients with high risk of nodal disease were included. Anatomical and T2*-weighted MR imaging was performed at 3T and at 7T (Magnetom® Prisma-fit and Magnetom® 7T, Siemens Healthcare, Erlangen, Germany), 24-36 hours after intravenous administration of Ferumoxtran‐10. Ferumoxtran-10 (Ferrotran, SPL Medical BV, Nijmegen, The Netherlands) is available for clinical studies and on terms of Named-Patient-Use Programs in the Netherlands and in Switzerland, and a large phase III international (Netherlands, Switzerland and Germany) multicenter pivotal trial has recently started.This study was approved by the institutional review and written informed consents were obtained from all patients. Patients were scanned in supine, feet first position. The scanned area contained at least the area from the aorta bifurcation to the base of the bladder (Table 1 for parameters). All studies were evaluated by two readers (TH and AF) after anonymization and randomization. The 3T studies were evaluated first, 7T studies followed a few months later. Nodal detection and annotation was performed while viewing both the anatomical as well as the T2*-weighted 3D datasets in any chosen orientation and with optional maximum intensity projections. Lymph nodes were scored on a 5 point Level of Suspicion (LoS) scale (metastases very unlikely (1), unlikely (2), equivocal (3), likely (4) and very likely (5)) depending on anatomical appearance and signal intensity on T2*-weighted MRI. Nodal annotations from two readers were separate entries in the viewer that could be turned on and off over the images of the patient, enabling very precise correlation between readers annotations. Correlation of annotations and nodal size measurements were performed by an independent reader (AV).
Results
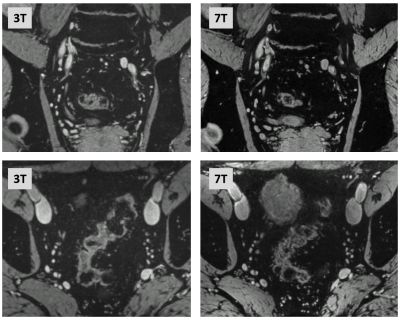
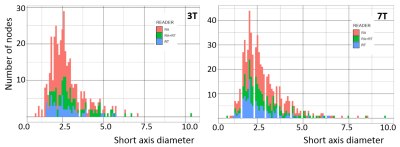
All 20 patients successfully underwent both scans without any adverse events (example in Fig.1). Reader A (RA) and reader T (RT) both annotated more lymph nodes on 7T MRI (476 and 284) compared to 3T MRI (345 and 164, respectively). Together, both readers identified more nodes than either reader alone with 99/410 co-identified nodes at 3T and 159/601 co-identified nodes at 7T. Both readers had a high intra-observer reliability, with RA scoring generally at a higher LoS than RT. LoS agreement between readers of co-identified nodes was fair on 3T MRI and moderate on 7T MRI (Table 2 confusion matrices). On both field strengths readers annotated lymph nodes of very small short axis diameters, which did not differ with field strength (Fig.2). Nodes observed by both readers tended to be somewhat larger at both field strengths. Median short axis diameters of all annotated lymph nodes at 3 and 7T were 2.6 and 2.8 mm. The short axis diameter of the nodes did not differ between LoS score, except for LoS5, which was significantly different from LoS4 and LoS3 at 7T (Dunn’s multiple comparison test after Kruskal Wallis non-parametric ANOVA test) (Fig.3).Discussion
In this first comparison of in vivo pelvic lymph node assessment between 3 and 7T it was clear that more suspicious lymph nodes were annotated on 7T MRI by both readers. Although both readers identified a very different amount of lymph nodes with only 25% concordance, they both annotated more suspicious nodes at higher field strength. Only LoS5 nodes at 7T were larger than LoS3 and LoS4 nodes at 7T, but overall no size relation with LoS was found. Even larger nodes at 7T were often not seen at 3T. From this work it is clear that suspicious nodes in prostate cancer are small, and that an ultra-high field strength can further improve visibility of lymph nodes.Conclusion
This first in vivo body MRI comparison of lymph node assessment with Ferumoxtran-10 between 3 and 7T translates the increased spatial resolution enabled by the sensitivity of an ultra-high magnetic field strength into a clinically relevant increased depiction of more suspicious lymph nodes in patients with advanced prostate cancer. Although annotating lymph nodes is not an easy task, 7T improves the interobserver agreement in scoring suspicious nodes.Acknowledgements
No acknowledgement found.References
1. Fossati N, Willemse P, Broeck T, et al. The benefits and harms of different extents of lymph node dissection during radical prostatectomy for prostate cancer: a systematic review. Eur Urol. 2017;72(1):84-109.
2. Preisser F, van den Bergh R, Gandaglia G, et al. Effect of extended pelvic lymph node dissection on oncologic outcomes in patients with D’Amico intermediate and high risk prostate cancer treated with radical prostatectomy: a multi-institutional study. J Urol. 2020;203(2):338-343.
3. Harisinghani M, Barentsz J, Hahn P, et al. Noninvasive detection of clinically occult lymph node metastases in prostate cancer. N Engl J Med. 2003;348(25):2491-2499.
4. Fortuin A, Deserno W, Meijer H, et al. Value of Pet/CT and MR lymphography in treatment of prostate cancer patients with lymph node metastases. Int J Radiat Oncol Biol Phys. 2012;84(3)712-718.
5. Heesakkers R, Jager G, Hövels A, et al. Prostate cancer: detection of lymph node metastases outside the routine surgical area with ferumoxtran-10-enhanced MR imaging. Radiology. 2009;251(2):408-414.
6. Heesakkers R, Fütterer J, Hövels A, et al. Prostate cancer evaluated with ferumoxtran-10-enhanced T2*-weighted MR imaging at 1.5 and 3.0T: early experience. Radiology. 006;239(2):481-487.
7. Philips BWJ, Fortuin AS, Orzada S, Scheenen TWJ, Maas MC. High resolution MR imaging of pelvic lymph nodes at 7 Tesla. Magn Reson Med 2017;78(3):1020-1028.
Figures