0010
Multi-Band Multi-Slab 3D Multi-Echo Acquisition for Simultaneous Time-of-Flight MR Angiography and Susceptibility-Weighted Imaging at 3T1Radiology and Biomedical Imaging, University of California, San Francisco, San Francisco, CA, United States, 2Applications and Workflow, GE Healthcare, Menlo Park, CA, United States, 3UCSF-UC Berkeley Graduate Program in Bioengineering, University of California, San Francisco and University of California, Berkeley, San Francisco, CA, United States
Synopsis
A single scan of multi-slab, multi-echo acquisition can simultaneously provide 3D time-of-flight (TOF) MR angiography and susceptibility-weighted imaging (SWI) MR venography, which allows for the assessment of vascular injury in the form of cerebral microbleeds in association with arteries and veins. However, the acquisition for high-resolution multi-slab 3D TOF-MRA/SWI with whole brain coverage takes over 10 minutes to acquire at 3T. In this work, we developed a 3D multi-slab, multi-echo acquisition for TOF-MRA/SWI with multi-band acceleration to reduce acquisition time and compared the resulting TOF-MRA and SWI images in patients with radiation-induced microbleeds.
Introduction
Radiation therapy (RT) is a widely utilized treatment for patients with gliomas1; however, RT can result in collateral injury to normal-appearing brain tissue, in the formation of small chronic brain hemorrhages called cerebral microbleeds (CMBs).2-3 The ability to assess characteristics of CMBs in conjunction with the surrounding arterial and venous vasculature would help to identify underlying vascular injury. A multi-slab, multi-echo acquisition to simultaneously provide 3D time-of-flight (TOF) MR angiography (MRA) and susceptibility-weighted imaging (SWI) MR venography has been suggested as an effective clinical tool in quantitative evaluation of radiation-induced vascular injury.4-6 However, the acquisition for high-resolution multi-slab 3D TOF-MRA/SWI with whole brain coverage takes over 10 minutes to acquire at 3T. In this work, we added multi-band (MB) acceleration7 to a 3T multi-echo TOF-MRA/SWI sequence to reduce acquisition time and applied to patients with radiation-induced microbleeds.Methods
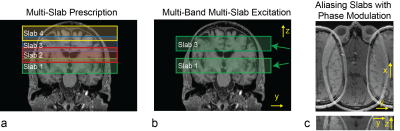
Sequence: A 3D multi-slab, multi-echo sequence for TOF-MRA/SWI was implemented for a GE 3T Signa Premier scanner (GE Healthcare, Waukesha, WI) by modifying a commercially available 3D multi-slab, single-echo TOF sequence based on multiple overlapping thin 3D slab acquisition (MOTSA)8 (Figure 1). Six additional echoes were added for SWI imaging with partial flow compensation incorporated in the readout direction.4-5 For the simultaneous excitation of two slabs, an original tilted optimized non-saturating ramp excitation pulse9 was frequency-modulated to match each slab location, and two modulated RF pulses were added together. Controlled aliasing in parallel imaging results in higher acceleration (CAIPIRINHA) was applied by independently modulating the phase of each RF pulse on both kz and ky phase encoding axes, in order to provide improved g-factors for MB reconstruction.10-11Patients & Data Acquisition: Three patients originally diagnosed with high-grade gliomas and had known radiation-induced microbleeds were scanned with original, no MB-accelerated TOF-MRA/SWI sequence and MB-accelerated TOF-MRA/SWI sequence on GE 3T Signa Premier scanner (GE Healthcare, Waukesha, WI) using a 48-channel phased-array brain coil. Imaging parameters used were 24x18 cm2 FOV, 384 x 288 matrix size, 1 mm slice thickness, 39 ms TR, ±41.67 kHz readout bandwidth, TEs of 2.3/8.23/10.43/16.37/18.56/24.5/26.7 ms, 66% partial kx readout, 20° flip angle, four axial slabs, 32 slices within each slab, and 6 overlapping slices between adjacent slabs. In-plane acceleration by a factor of 2 was also applied in the ky direction. Two TOF-SWI acquisitions, without and with MB acceleration, were performed for 10 minutes and 5 minutes, respectively. An extra calibration scan was conducted before TOF-MRA/SWI acquisitions for MB reconstruction.
Reconstruction: Image reconstruction was conducted offline using MATLAB. For data without MB acceleration, raw k-space data was first Fourier-transformed in the z direction, and for each slice, in-plane ARC reconstruction12 and partial Fourier reconstruction with a projection onto convex sets (POCS) algorithm13 were applied. For data with MB acceleration, slice GRAPPA reconstruction was additionally applied to unalias two superimposed slices14 after in-plane ARC reconstruction. After reconstructing complex images for each coil, images from the four slabs were concatenated. A composite SWI image was attained from the 2nd to 7th echo images after creating the high-pass filtered phase image using a 2D Hanning filter and SWI image for each echo.4,6
Results and Discussion
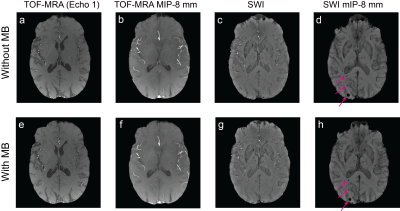
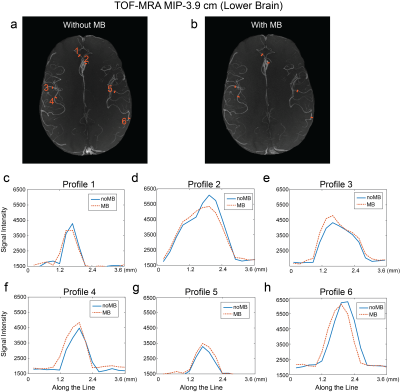
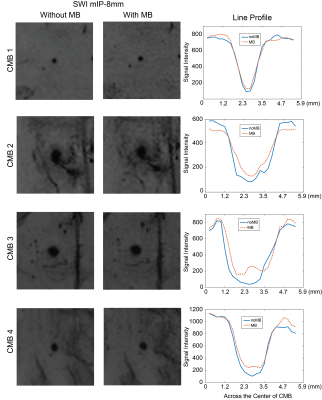
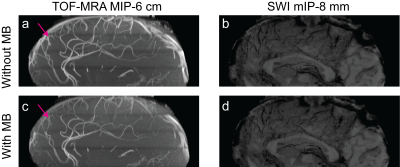
Figure 2 demonstrates the first echo images for TOF-MRA, the maximum intensity projection (MIP) of TOF-MRA images over the thickness of 8 mm (TOF-MRA MIP-8 mm images), composite SWI images, and the minimum intensity projection (mIP) of composite SWI images over the thickness of 8 mm (SWI mIP-8 mm images), from original and MB-accelerated images from one patient. No visible aliasing artifacts were observed even though MB-accelerated images had slightly lower SNR. From SWI mIP-8 mm images, radiation-induced CMBs (depicted by arrows) were clearly visible on both acquisitions. To further assess the difference in arterial and CMB contrasts from two acquisitions, line profiles across arteries and CMBs were compared between the two acquisitions, after resampling images with in-plane pixel size to 0.234x0.234 mm2. Figure 3 shows line profiles across six arteries over TOF-MRA MIP images (over 3.9 cm thick inferior brain) from another patient; Figure 4 shows line profiles across four CMBs detected from the two patients on SMI mIP-8 mm images. The two figures illustrated that arterial and CMB contrasts from both acquisitions were similar, indicating MB acceleration would not diminish the ability to detect vessels and CMBs.Figure 5 shows TOF-MRA MIP-6 cm images and SWI mIP-8mm images from the central brain after sagittally-reformatting from both acquisitions (patient shown in Figure 3). Arteries and veins were well-visualized with either TOF-MRA MIP or SWI-mIP images; however, MB acceleration slightly reduced arterial signal in the upper slabs of the TOF-MRA, probably due to insufficient time to recover to full magnetization in flowing spins after being partially saturated while transversing the other excited slab below.
Conclusion
This work demonstrates that MB acceleration can be combined with multi-slab 3D TOF-MRA/SWI to reduce acquisition time without degrading depiction of vessel/CMB contrasts or yielding visible aliasing artifacts. Future work will further optimize the acquisition and post-processing pipelines to recover arterial signal in the upper-most slabs and to improve overall MB-accelerated image quality.Acknowledgements
This work was supported by a technology development research grant from GE Healthcare.References
1. Laperriere N, Zuraw L, Cairncross G. Radiotherapy for newly diagnosed malignant glioma in adults: a systematic review. Radiother Oncol 2002;64:259–273.
2. Valk PE, Dillon WP. Radiation injury of the brain. AJNR Am J Neuroradiol 1991;12(1):45-62.
3. Lupo JM, Chuang CF, Chang SM, Barani IJ, Jimenez B, Hess CP, Nelson SJ. 7-Tesla susceptibility weighted imaging to assess the effects of radiotherapy on normal-appearing brain in patients with glioma. Int J Radiat Oncol Biol Phys 2012;82(3):e493–500.
4. Bian W, Banerjee S, Kelly DA, Hess CP, Larson PE, Chang SM, Nelson SJ, Lupo JM. Simultaneous imaging of radiation-induced cerebral microbleeds, arteries and veins, using a multiple gradient echo sequence at 7 Tesla. J Magn Reson Imaging 2015; 42(2):269-79.
5. Du YPP Jin ZY, Hu YZ, Tanabe J. Multi-Echo Acquisition of MR Angiography and Venography of the Brain at 3 Tesla. J Magn Reson Imaging 2009;30(2):449-454.
6. Zou X, Bian W, Tamir JI, Banerjee S, Chang SM, Lustig M, Nelson SJ, and Lupo JM. Application of 3D High-resolution Multi-echo TOF-SWI Acquisition in Radiation-induced Cerebral Microbleeds at 3T, In: Proceedings of the 23rd Annual Meeting of ISMRM, Toronto, Ontario, Canada, p. 66.
7. Larkman DJ, Hajnal JV, Herlihy AH, Coutts GA, Young IR and Ehnholm G. Use of multicoil arrays for separation of signal from multiple slices simultaneously excited. J Magn Reson. Imaging 2001;13:313-331.
8. Parker DL, Yuan C, Blatter DD. MR angiography by multiple thin slab 3D acquisition. Magn Reson Med 1991;17(2):434-451.
9. Atkinson D, Brant-Zawadzki M, Gillan G, Purdy D, and Laub G. Improved MR angiography: magnetization transfer suppression with variable flip angle excitation and increased resolution. Radiology 1995;190(3):890-894.
10. Breuer FA, Blaimer M, Heidemann RM, Mueller MF, Griswold MA, and Jakob PM. Controlled aliasing in parallel imaging results in higher acceleration (CAIPIRINHA) for multi‐slice imaging. Magn Reson Med 2005;53(3):684-691.
11. Hargreaves BA, Cunningham CH, Pauly JM, and Daniel BL. Independent phase modulation for efficient dual‐band 3D imaging. Magn Reson Med 2007;57(4):798-780.
12. Beatty PJ, Brau AC, Chang S, Joshi SM, Michelich CR, Bayram E, Nelson TE, Herfkens RJ, Brittain JH. A method for autocalibrating 2-D accelerated volumetric parallel imaging with clinically practical reconstruction times. In: Proceedings of the 15th Annual Meeting of ISMRM, Berlin, Germany, 2007. p. 1749.
13. Haacke EM, Lindskog ED, Lin W. A Fast, Iterative, Partial-Fourier Technique Capable of Local Phase Recovery. J Magn Reson 1991;92(1):126-145.
14. Setsompop K, Gagoski BA, Polimeni JR, Witzel T, Wedeen VJ, Wald LL. Blipped-controlled aliasing in parallel imaging for simultaneous multislice echo planar imaging with reduced g-factor penalty. Magn Reson Med 2012;67(5):1210-1224.
Figures