0009
Whole-heart CMRA non-rigid motion compensation with autofocus virtual 3D iNAV1School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom, 2MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom
Synopsis
3D whole-heart coronary MR angiography (CMRA) acquisition remains lengthy and can suffer from residual motion and/or undersampling related artifacts. 2D image-navigator based non-rigid respiratory motion compensation has been recently proposed to accelerate the CMRA scan. This framework combines 2D beat-to-beat translational and 3D bin-to-bin non-rigid motion correction. However, beat-to-beat anterior-posterior motion is not corrected for with this approach, which can result in significant residual motion. Here we propose a virtual 3D iNAV approach that exploits autofocus motion correction to further enable beat-to-beat anterior-posterior translational motion correction, assuming a linear relationship between the translational foot-head and anterior-posterior movement of the heart.
Introduction
3D whole-heart coronary MR angiography (CMRA) is a promising tool for non-invasive visualization of cardiac anatomy and assessment of coronary artery integrity. Despite several improvements, CMRA acquisition remains lengthy and can suffer from residual motion and/or undersampling related artifacts. Accelerated non-rigid motion compensated free-breathing 3D whole-heart imaging1,2 enables 100% respiratory scan efficiency and predictable scan time. This approach is based on low resolution 2D image navigators (iNAVs)3 acquired at every heart beat that enable beat-to-beat translational respiratory motion correction in the foot-head (FH) and right-left (RL) directions, combined with 3D non-rigid motion compensation in FH, RL and anterior-posterior (AP) directions on a bin-to-bin basis. However, beat-to-beat AP motion is not corrected in this approach and can result in significant residual motion. Here we propose to further correct for beat-to-beat AP motion by introducing a novel virtual 3D iNAV approach that exploits autofocus4 motion correction in AP and RL directions, assuming a linear relationship between the translational FH and AP movement of the heart5,6. The virtual 3D iNAV was incorporated in the non-rigid motion compensation CMRA framework and was evaluated on 5 patients with known or suspected cardiovascular disease.Methods
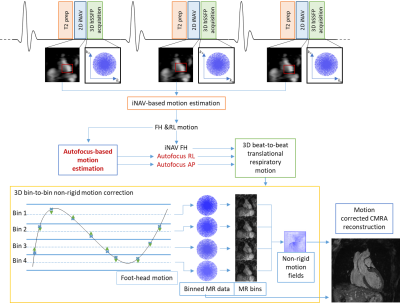
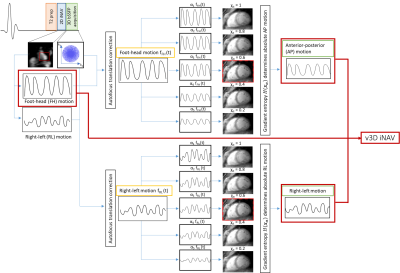
Acquisition & Reconstruction:Free-breathing 3D whole-heart CMRA was acquired using a 3-fold undersampled variable-density Cartesian trajectory7 (Figure 1). Virtual 3D iNAV translational motion estimation is performed sequentially for each spatial dimension (Figure 2). Beat-to-beat 3D translational respiratory motion is estimated in FH from the 2D iNAVs and in RL and AP directions from the autofocus approach (Figure 1). RL motion is proportional to the RL iNAV signal (fRL(t)), while the AP motion is assumed to be proportional to the FH iNAV signal, fFH(t), similar to previous work5,6. A set of translationally corrected images (𝒙𝜶) are obtained by correcting the data with different motion signals αf(t) in RL and later in AP directions. The optimal scaling α is obtained by minimizing the localized gradient entropy $$H(x_α)=-Σ_ih_α(x_α(i))log_2h_α(x_α(i))$$ in a subject varying region of interest surrounding the left ventricle, where ℎ𝛼 is the normalized spatial gradient and 𝒙𝜶(𝑖) is the 𝑖th pixel intensity8. This virtual 3D iNAV is then used to bin (FH iNAV) and motion correct the data (v3D iNAV), producing respiratory-resolved images with intra-bin 3D translational motion correction. 3D non-rigid motion is then estimated from the respiratory-resolved bin images (via image registration) and incorporated into a motion-compensated reconstruction9 to produce the final motion-corrected CMRA datasets.
Imaging & Analysis:
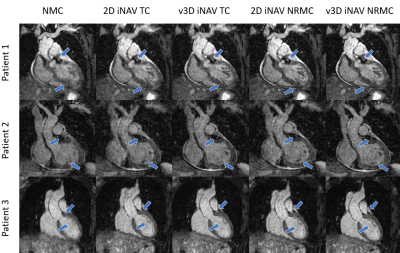
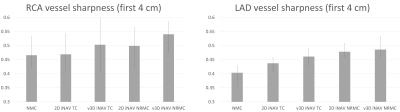
The proposed reconstruction using the virtual 3D iNAV approach was investigated in free-breathing 3D CMRA images acquired at 1.5 T system (Magnetom Aera, Siemens Healthcare AG, Germany). The framework was tested in 5 patients (2 males, 46±10 years-old) with known or suspected cardiovascular disease. Relevant CMRA parameters include: 3D bSSFP, TR/TE=3.35/1.47 ms, FA=90°, T2-preparation=40 ms, 3-fold undersampling, 1.2 mm3 isotropic resolution, acquisition time=6.1±0.5 min. A subject-specific trigger delay and acquisition window were set to coincide with the mid-diastolic rest period. Same FOV with FA=3º was used for the iNAV. Each dataset was reconstructed (a) with no motion correction (NMC), (b) with 2D iNAV translational correction only (2D iNAV TC), (c) with v3D iNAV translation correction only (v3D iNAV TC), (d) with 2D iNAV non-rigid motion correction (2D iNAV NRMC) as previously proposed2 and (e) with the proposed v3D iNAV for 3D beat-to-beat translational and 3D bin-to-bin non-rigid motion correction (v3D iNAV NRMC). The 3D CMRA images were reformatted to visualise both the left anterior descending (LAD) and right (RCA) coronary arteries simultaneously. Vessel sharpness in the first 4 cm was computed for both coronary arteries.
Results
Virtual 3D iNAV-based non-rigid motion compensated images were compared against NMC, 2D iNAV TC, v3D iNAV TC and 2D iNAV NRMC images. Improvements (in some subjects subtle) due to virtual 3D iNAV NRMC can be observed in most cases both in coronal view and in reformatted images (arrows in Figure 3 and Figure 4). This was also observed quantitatively when comparing the vessel sharpness in the RCA and LAD (Figure 5). On average, v3D iNAV NRMC vessel sharpness of RCA was 54±5% compared to 50±7% with 2D iNAV NRMC. Vessel sharpness of LAD for v3D iNAV was 49±5% compared to 48±3% with 2D iNAV NRMC (vessel sharpness of first 4 cm – NMC: RCA = 47±7%, LAD = 40±3%; TR 2D iNAV: RCA = 47±7%, LAD = 44±2%; TR v3D iNAV: RCA = 50±10%, LAD = 46±3%).Conclusion
Here we introduce a method for virtual 3D iNAV based non-rigid motion-compensated reconstruction that further includes beat-to-beat AP translational motion correction for whole-heart CMRA imaging. Visible improvements were observed with the virtual 3D iNAV-based motion reconstruction in comparison to the 2D iNAV-based approach. Vessel sharpness in the first 4 cm improved in both LAD and RCA with v3D iNAV NRMC in all cases, with different impact depending on the case. Further studies will investigate this approach in a larger cohort of patients with coronary artery disease.Acknowledgements
This work was supported by EPSRC (EP/L015226/1, EP/P032311/1, EP/P007619/1 and EP/P001009/1) and the Wellcome/EPSRC Centre for Medical Engineering (NS/A000049/1).References
1. Munoz, C., Cruz, G., Neji, R., Botnar, R. M. & Prieto, C. Motion corrected water/fat whole-heart coronary MR angiography with 100% respiratory efficiency. Magn. Reson. Med. 82, 732–742 (2019).
2. Cruz, G., Atkinson, D., Henningsson, M., Botnar, R. M. & Prieto, C. Highly efficient nonrigid motion-corrected 3D whole-heart coronary vessel wall imaging. Magn. Reson. Med. 77, 1894–1908 (2017).
3. Henningsson, M. et al. Whole-heart coronary MR angiography with 2D self-navigated image reconstruction. Magn. Reson. Med. 67, 437–445 (2012).
4. Atkinson, D. et al. Automatic compensation of motion artifacts in MRI. Magn. Reson. Med. 41, 163–170 (1999).
5. Cruz, G. et al. 3D free-breathing cardiac magnetic resonance fingerprinting. NMR Biomed. 33, e4370 (2020).
6. Cheng, J. Y. et al. Nonrigid motion correction in 3D using autofocusing withlocalized linear translations. Magn. Reson. Med. 68, 1785–1797 (2012).
7. Prieto, C. et al. Highly efficient respiratory motion compensated free-breathing coronary mra using golden-step Cartesian acquisition. J. Magn. Reson. Imaging 41, 738–746 (2015).
8. Ingle, R. R. et al. Nonrigid autofocus motion correction for coronary MR angiography with a 3D cones trajectory. Magn. Reson. Med. 72, 347–361 (2014).
9. Roy, C. W. et al. Motion Compensated Coronary MRA using Focused Navigation (fNAV). ISMRM 2020, Abstract number 1321.
Figures