S99
Operating a Hybrid PET/MR Scanner: Challenges and Opportunities
Dawn Holley1, Kim Halbert1, and Mehdi Khalighi1
1Radiology, Stanford University, Stanford, CA, United States
1Radiology, Stanford University, Stanford, CA, United States
Synopsis
Simultaneous PET/MR imaging is still a relatively new dual modality. As such, unique challenges are commonly faced across departments. What were once commonly separate, Nuclear Medicine and Radiology departments now need to work together to create new workflows, protocols and management systems. Questions commonly arise regarding how these two modalities and departments can best come together for management success. A survey of 19 questions was distributed to 12 different PET/MR departments in order to gain an understanding of what challenges are often faced and how to resolve them, as well as any commonalities across successful departments.
Background
Simultaneous PET/MR imaging is still a relatively new dual modality. As such, unique challenges are commonly faced across departments. What were once commonly separate, Nuclear Medicine and Radiology departments now need to work together and create new workflows, protocols and management systems. Questions commonly arise regarding who is qualified to operate the system, how are technologists cross trained for each modality, how can a department generate physician buy-in for referral scans and how can the two modalities and departments best come together for management success.Communication across departments is still relatively uncommon, leaving most sites to work through these challenges by costly trial and error. The ISMRM/SNMMI supported PET/MR workshop has been a successful first step in bridging the communication gap between PET/MR sites and building a supportive community.
While PET/MR community wide communication is fundamental to highlighting common challenges unique to operating a successful PET/MR department, to date it has been limited and informal. The goal of this research is to survey many departments and highlight common challenges faced and how they have been successfully overcome.
An overview of successful management operations can act as a valuable resource for new or existing departments that are struggling to navigate this new modality.
Methods
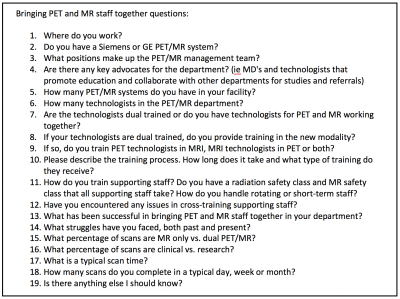
A survey of 19 questions, provided in Figure 1, was sent to managing PET/MR technologists across 12 institutions.Responses to the survey were reviewed and similarities were highlighted.
Results
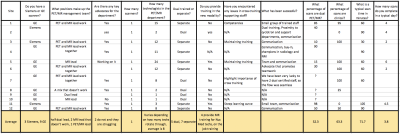
Participating institutions include 11 PET/MR departments across the US and 1 PET/MR department in Canada. Of these sites, 9 departments use a GE Signa PET/MR and 3 departments use a Siemens mMR. All departments operate a single PET/MR system. Five of the departments have dual certified PET and MR technologists, the other 7 utilize PET technologists to handle injection of radioactive isotopes and image reconstruction, and MR technologists to conduct the imaging. Of these 5 departments, 4 offer concurrent MRI training to PET technologists. Of note, 6 departments have both a PET and an MR technologist lead manager that work together to manage the department.All but 2 departments claim to have at least one key advocate that helps to oversee the department and reach out to educate referring physicians and research teams.
All sites offer MRI safety training to Nuclear Medicine staff and radiation safety training to MRI staff. Struggles with cross training include maintaining current training and emphasizing the importance of safety training.
Across all sites, about half the scans are dual PET/MR, as opposed to using the PET/MR for MR only. Just over 63% are clinical rather than research. Scan times for PET/MR average just over an hour and there are between 3-4 scans completed in a day. Many sites fill open schedule time with MR only clinical scans.
In reviewing responses, technologists reported 4 main commonalities which contribute to a successful department. They all had at least one strong department advocate, open communication between department staff and supporting Nuclear Medicine and Radiology departments, a clear sense of department teamwork and many also benefited from the support of a larger, world-wide PET/MR community.
Conclusion
A review of the survey responses uncovered an understanding of the necessity for each of the 4 key components within each successful department.A strong department advocate is typically a physician that supports the PET/MR department as both a role model for the team and collaborator to generate physician buy-in. This buy-in leads to new research studies or referrals for the PET/MR, but it also helps Nuclear Medicine and Radiology staff come together and communicate as a team. The departments that did have physicians and manager advocates were more excited, proud and happy to answer survey questions and discuss their department.
A clear commonality across all successful departments was open communication. Since it is still uncommon in the United States for PET technologists to receive training and certification in MRI, many departments require separate PET and MR technologists to operate the system together. Additionally, the most successful management teams comprise of two lead technologists, one from Nuclear Medicine and one from Radiology. Without each, the unique protocol and workflow needs are not fully understood or supported.
Since it takes more staff to manage and operate a PET/MR hybrid system, a clear sense of teamwork was also important. Each department that reported a strong sense of teamwork and unity also had a strong physician advocate, acting as a champion for the department and creating buy-in, and a resulting sense of excitement for the modality.
Finally, almost every participating department reported a perceived benefit to open communication and sense of unity across all PET/MR sites. The need to continue to build and strengthen this community with collaborative meetings and workshops is likely beneficial to the success of new PET/MR departments.