S87
Analysis on breast tumor movement using MRIs scanned in prone and supine positions
chuan bing wang1 and da peng li2
1Department of Radiology, the First Affiliated Hospital of Nanjing Medical University (Jiangsu Province Hospital), Nanjing, China, 2the First Affiliated Hospital of Nanjing Medical University (Jiangsu Province Hospital), nan jing, China
1Department of Radiology, the First Affiliated Hospital of Nanjing Medical University (Jiangsu Province Hospital), Nanjing, China, 2the First Affiliated Hospital of Nanjing Medical University (Jiangsu Province Hospital), nan jing, China
Synopsis
The aim of this study is to evaluate the volume change of breast tumor, various kinds ofspatial movementin nipple and the bottom center of the sternum origin, and distance from tumor center to the chest wall from prone to supine MRIs, and then to predict more accuracy tumor positions for surgical planning in the operation room.
Background or Purpose
To quantitatively evaluate breast tumor mobility and shape changes by posture changes using prone and supine magnetic resonance imaging (MRIs)for breast conservation surgery (BCS).Methods
Thirty one patients who were diagnosed with breast cancer and scheduled to receive neoadjuvant systemic therapy (NST) under the plan for BCS were studied.After MRIscanning on prone position, mDIXONscan on supine position was performed immediately.Based on tumor segmentation,every tumors’ volume and position were evaluated in both positions.The volume change of breast tumor, various kinds of spatial movement in nipple and the bottom center of the sternum origin, and distance from tumor center to the chest wallwere also measured and analyzed.Results
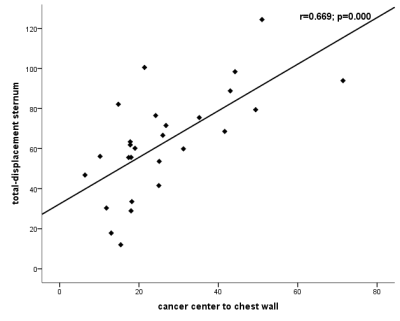
The mean and standard deviation tumor volumes of prone and supine were 9797.3±9390.6, 9795.5±9413.1 mm³, respectively and no significant difference was found between two positions (p=0.877). The average tumor movement at the nipple origin from prone to supine position was 27.8±3.3mm. Total movement from prone to supine position at the bottom center of the sternumorigin was 63.1±26.2 mm which was strongly correlated with the distance from tumor center to chest wall (r=0.669; p<0.05).Conclusions
Tumor change from prone to supine position at the nipple origin differs depending on tumor location in the breast, and their average total distances were no more than 30 mm in Asian population. However, prone-to-supine movement of all tumors at the bottom center of the sternum origin tend to move outward from the sagittal centerline of the body on coronal plane, move to the inside of body on sagittal plane and move to the outward and downward closed to the body on axial plane.The results of above might be helpful for surgeons using standard prone position MR image to localize the tumor position in the operating room.Acknowledgements
We thank Department of breast Surgery,for give us breast cancer patients information of this manuscript.References
1. Melloni, P. and R. Valls, The use of MRI scanning for investigating soft-tissue abnormalities in the elbow. Eur J Radiol, 2005. 54(2): p. 303-13.2. Howarth, S.P., et al., Non-invasive MR imaging of inflammation in a patient with both asymptomatic carotid atheroma and an abdominal aortic aneurysm: a case report. Ann Surg Innov Res, 2007. 1: p. 4.3. Waljee, J.F., et al., Predictors of re-excision among women undergoing breast-conserving surgery for cancer. Ann Surg Oncol, 2008. 15(5): p. 1297-303.4. Solin, L.J., et al., Relationship of breast magnetic resonance imaging to outcome after breast-conservation treatment with radiation for women with early-stage invasive breast carcinoma or ductal carcinoma in situ. J Clin Oncol, 2008. 26(3): p. 386-91.5. Pengel, K.E., et al., The impact of preoperative MRI on breast-conserving surgery of invasive cancer: a comparative cohort study. Breast Cancer Res Treat, 2009. 116(1): p. 161-9.6. Houssami, N., et al., An individual person data meta-analysis of preoperative magnetic resonance imaging and breast cancer recurrence. J Clin Oncol, 2014. 32(5): p. 392-401.7. Sung, J.S., et al., Preoperative breast MRI for early-stage breast cancer: effect on surgical and long-term outcomes. AJR Am J Roentgenol, 2014. 202(6): p. 1376-82.8. Morris, E.A., Should we dispense with preoperative breast MRI? The Lancet, 2010. 375(9714): p. 528-530.9. Telegrafo, M., et al., Supine breast US: how to correlate breast lesions from prone MRI. Br J Radiol, 2016. 89(1059): p. 20150497.10. Pogson, E.M., et al., Comparison of Magnetic Resonance Imaging and Computed Tomography for Breast Target Volume Delineation in Prone and Supine Positions. Int J Radiat Oncol Biol Phys, 2016. 96(4): p. 905-912.11. Satake, H., et al., Prediction of prone-to-supine tumor displacement in the breast using patient position change: investigation with prone MRI and supine CT. Breast Cancer, 2016. 23(1): p. 149-58.12. Park, V.Y., et al., Second-Look US: How to Find Breast Lesions with a Suspicious MR Imaging Appearance. Radiographics, 2013. 33(5): p. 1361-1375.13. LaTrenta, L.R., et al., Breast lesions detected with MR imaging: utility and histopathologic importance of identification with US. Radiology, 2003. 227(3): p. 856-61.14. Carbonaro, L.A., et al., Contrast enhanced breast MRI: spatial displacement from prone to supine patient's position. Preliminary results. Eur J Radiol, 2012. 81(6): p. e771-4.15. Gombos, E.C., et al., Intraoperative Supine Breast MR Imaging to Quantify Tumor Deformation and Detection of Residual Breast Cancer: Preliminary Results. Radiology, 2016. 281(3): p. 720-729.16. Nakamura, R., et al., Breast-conserving surgery using supine magnetic resonance imaging in breast cancer patients receiving neoadjuvant chemotherapy. Breast, 2008. 17(3): p. 245-51.17. Siegler, P., et al., Supine breast MRI. J Magn Reson Imaging, 2011. 34(5): p. 1212-7.18. Intraoperative supine breast MRimaging to quantify tumor deformation and detection of residual breast cancer.pdf. 2016.19. Samani, A., J. Zubovits, and D. Plewes, Elastic moduli of normal and pathological human breast tissues: an inversion-technique-based investigation of 169 samples. Phys Med Biol, 2007. 52(6): p. 1565-76.Figures
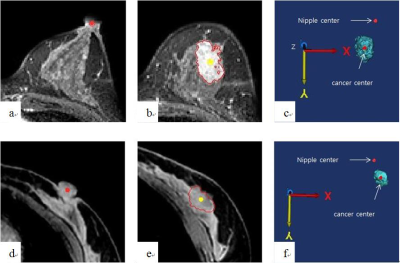
Nipple and tumorcenter in three-dimensional coordinateswere visualized. a-c)prone position.
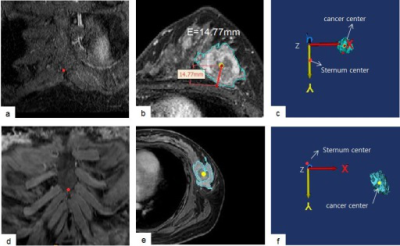
The bottom center of the sternum andtumor center in 3D coordinateswere obtained
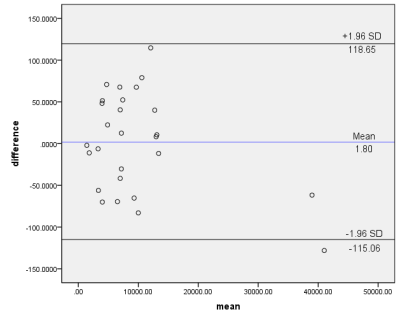
27 patients tumor volume of prone and supine position measurement.
X-Z (coronal plane)and X-Y (axial plane)viewof the bilateral breasts after fixing the nipple asthe origin (0, 0).
X-Z, Y-Z and X-Y viewof the bilateral breasts after fixing the bottom center of the sternumasthe origin (0, 0).

correlationof total tumor movementat the nipple originwith the distance from tumor center to chest wall (r=0.669; p<0.05).
correlationof total tumor movementat the bottom center of the sternumorigin with the distance from tumor center to chest wall (r=0.072; p=0.721).