S71
Optimization of Metal Artifact Reduction (O-MAR) Imaging1Philips Healthcare, Gainesville, FL, United States, 23545 SW 47th Ave, Philips Healthcare, Gainesville, FL, United States
Synopsis
Patients with MR Conditional orthopedic implants can be challenging to scan due to susceptibility artifact from metal implants. Use of metal artifact reduction (MARS) techniques can help reduce signal loss from metal implants, however, are not usually sufficient to allow for detailed peri-prosthetic tissue visualization. Metal-induced field inhomogeneities cannot be accurately modeled, which is why O-MAR (MARS+VAT) can improve in-plane distortions by utilizing a more robust spatial encoding approach. Here we present the conceptual background behind the O-MAR technique and work done to provide guidance for optimized metal reduction imaging protocols.
Background
As life expectancy continues to increase, so does the number of patients receiving orthopedic implants1. Patients receiving orthopedic implants are at risk for developing: osteolysis, metallosis, heterotopic ossifiction, osteonecrosis, and component loosening2. MRI provides excellent soft-tissue contrast and is the modality of choice for the assessment for these clinical indications, but suffer from susceptibility artifacts3,4. Therefore, when imaging orthopedic implants with MRI steps need to be taken to reduce the metal artifact. Common approaches for reducing metal artifact include use of spin echo based sequences over gradient echo based sequences, reducing the echo spacing in the echo train of turbo spin echo sequences, and increasing the receiver bandwidth. The use of all three of these imaging strategies collectively is called MARS (Metal Artifact Reduction) and originally described by Olsen et. al (2000) but now commonly available from every vendor (Philips, Siemens, and GE). Improvements on MARS have taken place by adding view angle tilt (VAT)5,6 with MARS to further reduce in-plane susceptibility artifact and slice encoding for metal artifact correction (SEMAC)7 which also helps to reduce through-pane susceptibility artifact. On the Philips platform the MARS+VAT technique is called O-MAR (Orthopedic Metal Artifact Reduction). Here we present the conceptual background behind the O-MAR technique and work done to provide guidance for optimized metal reduction imaging protocols.O-MAR (MARS+VAT) Teaching Points
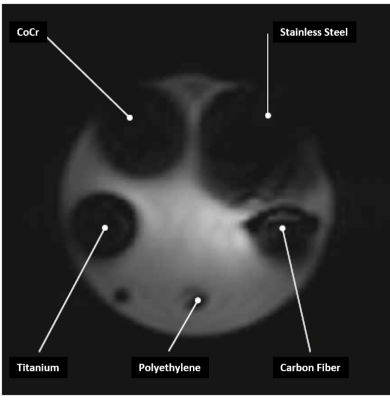
Implant: Severity of artifact caused by the implant depends on many factors including: implant material, size, shape, orientation, and the imaging sequence being used (Figure1).Susceptibility Artifact: The magnetic susceptibility of metal is much higher than that of tissue, such that around metal, very large variations in Larmor frequency occur. This not only causes signal reduction, but also signal loss. So called signal pile-ups can also occur due to non-linear frequency-position mapping. Slice profile selection also relies on local precession frequency variations and is equally affected by susceptibility variations, resulting in distorted slice profiles and consequently signal misregistration in the slice direction. Consequently, around metal implants, anatomy can be severely obscured.
Spin echo: Spin echo based sequences are less prone to metal artifacts compared to gradient echo based sequences because the 180˚ RF refocusing pulse causes signal loss at the rate of T2 compared to T2*.
Bandwidth: Geometric distortions are caused by altered Larmor frequencies around metal implants, so increasing the receiver bandwidth helps reduce the range of resonant frequencies over which the distortion is spread over the pixels and containing the in-plane geometric distortion to a smaller area. However, be aware that increasing receiver bandwidth reduces the signal-to-noise ratio (SNR), so care is need to find the optimal balance between SNR and artifact reduction.
Echo spacing: Reducing the echo spacing allows for a shorter minimum echo time (TE) and a shorter shot length. This is also usually achieved by increasing the receiver bandwidth. By decreasing the minimum TE, less dephasing due to the metal susceptibility occurs. Moreover, shortening the shot length by having a smaller echo spacing decreases the dephasing associated with the application of multiple phase encoding gradients in a TSE acquisition. However, image contrast needs to be considered when choosing the minimum TE and echo spacing as all effect the final image contrast.
Resolution: While not necessarily included in the MARS technique, increasing resolution also helps reduce metal artifacts by reducing geometric distortions similarly to increasing the receiver bandwidth.
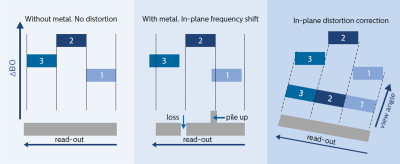
VAT: VAT is an efficient technique for in-plane artifact correction5. VAT uses an extra gradient in the slice select direction during the signal read-out, and the slice is effectively viewed from an angle (Figure 2). This VAT tilt works because the sum of artifacts from the frequency shifts in the slice select and the read-out direction caused by the metal results in a frequency shift with an oblique orientation. By tilting or using a read-out with an oblique angle the received signals can be projected into the correct pixel. VAT can cause blurring but this is minimized by the high receiver bandwidth already implemented by the MARS7.
Parallel Imaging: Use of parallel imaging is allowed with O-MAR in conjunction with parallel array coils. However, parallel imaging relies on the use of a reference scan to determine coil sensitivities that can lead to artifacts during image reconstruction.
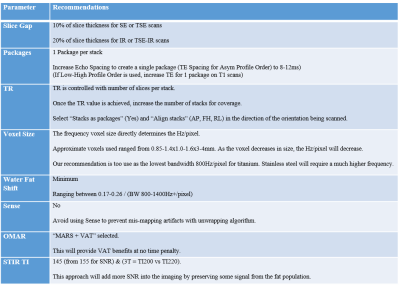
Additional O-MAR Parameter Optimization Considerations (Figure 3)
Summary
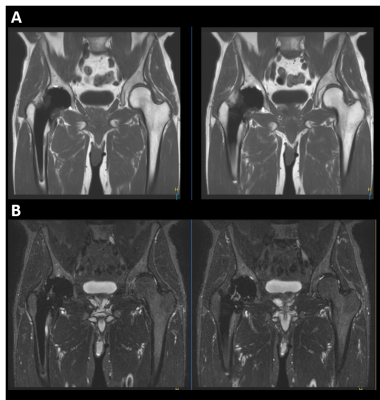
Patients with MR Conditional orthopedic implants can be challenging to scan due to susceptibility artifact from metal implants. Use of MARS techniques (TSE sequences with short echo spacing and high receiver bandwidth) can help reduce signal loss from metal implants, however, are not usually sufficient to allow for peri-prosthetic tissue visualization. Metal-induced field inhomogeneities cannot be accurately modeled, therefore O-MAR (MARS+VAT) which relies on a more robust spatial encoding approach should be implemented in the presence of metal implants to improve in-plane distortions. With O-MAR all relevant image contrasts can be obtained (T1, T2, PD, and STIR) at 1.5T and 3T filed strengths (Figure 4).Acknowledgements
No acknowledgement found.References
1. Kurtz, S., et al., Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am, 2007. (4): p. 780-785.
2. Ulrike Dapunt et al, HYPERLINK “/pmc/articles/ PMC3994416/”On the inflammatory response in metalon- metal implants , J Transl Med. 2014; 12: 74.
3. B.A. Hargreaves, P. W. Worters, K.B. Pauly, J.M.Koch and G.E. Gold, Metal-Induced artifacts in MRI, AJR: 197, sept 2011.
4. L.M. White, J.K. Kim, M. Mehta, N. Merchant, M.E. Schweitzer, W.B. Morrison, C.R. Hutchinson, A.E. Gross. Complications of total hip arthroplasty: MR imaging— initial experience. Radiology. 2000;215:254-62.
5. J.E.1 Vandevenne, F.M. Vanhoenacker, P.M. Parizel, K. Butts, J.M. Pauly, R.K. Lang. Reduction of metal artefacts in musculoskeletal MR imaging, JBR-BTR. 2007 Sep-Oct;90(5):345-9.
6. R.V. Olsen, P.L. Munk, M.J. Lee, et al.: Metal artifact reduction sequence: early clinical applications. Radiographics, 2000, 20: 699-712.
7. K. Butts, J.M. Pauly, G.E. Gold: Reduction of blurring in view angle tilting MRI. Magn Reson Med, 2005, 53: 418- 424..
Figures