S109
7T Knee MRI: Clinical Benefits and Challenges1Radiology, Stanford University School of Medicine, Stanford, CA, United States
Synopsis
Diagnostic MRI scanning of the knee at 3T offers multiple contrasts and definition of anatomical structures, presenting pathology, and allows quantitative performance methods. Ultra high field (7T) systems offer improved resolution and SNR for visualization of small morphological changes and translation of quantitative methods presents challenges in field uniformity and shading artifacts which limit the robustness and clinical potential of these systems.In this work we implement a new method to overcome field inhomogeneity errors and assess the potential clinical benefits of knee imaging at 7T.
Purpose
Knee injuries, chronic knee pain, and invading osteoarthritis (OA) are increasing in occurrence, resulting in over 2 million MRI exams performed in the United States each year(1, 2). Diagnostic MRI scanning at 1.5T and 3.0T is able to visualize anatomical injury and pathology of the knee and offers depiction of soft tissues with multiple contrasts as well as advanced quantitative methods to probe tissue microstructure(3), however limited SNR makes high-resolution scanning of small morphological changes challenging(4). Scanning the knee at 7T MRI systems offer improved resolution for detection of structural changes and translational of quantitative methods to detect the earliest biochemical changes in OA(5, 6). Although protocol development and applications have been limited at 7T due to lack of access of high field MRI as well as limited clinical potential, a new clinical approval by the US FDA and European CE for 7T knee imaging opening up the translational potential of these systems. In this work we assess the potential clinical benefits of knee imaging at 7T as well as challenges for imaging at ultra-high magnetic fields. In this work we assess the potential clinical benefits of knee imaging at 7T as well as challenges for imaging at ultra-high magnetic fields.Methods
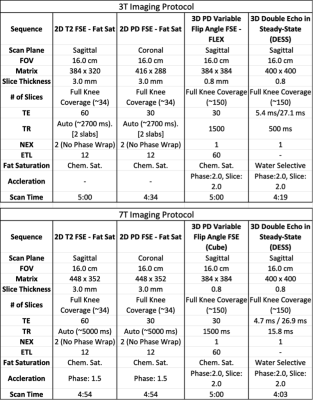
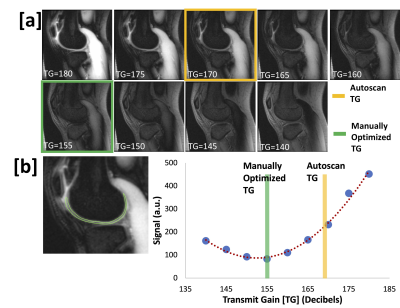
MRI exams were performed 6 healthy volunteers after informed consent on a 3T whole body scanner (GE Healthcare, Waukesha, WI) with a 16-channel phased array flexible knee coil (Neocoil, Pewaukee, WI) and 7T whole body scanner (GE Healthcare) with a 28-channel transmit-receive knee coil. The Neocoil flexible array coil was utilized at 3T due to improved signal-to-noise compared with a 18-channel transmit-receive coil. The imaging protocol is listed in table 1. In short, we aimed to utilize the increased SNR at 7T to push the resolution of both conventional 2D FSE sequences as well as the new 3D sequences that promise to speed up knee scanning by offering high-resolution images capable of reformatting into any scan plan.MRI scanning at 7T presents challenges and one of the biggest is the increased transmit field (B1) inhomogeneity. This presents as shading in images with higher signal in certain areas and lower signal in other areas, which can make interpretation of images difficult for clinicians. This also presents a challenge in determining the correct system transmit gain (TG) to ensure that signal (flip angles) in the tissues of interest are optimized. To better determine the optimal transmit gain and minimize shading in tissues of interest, we created a sequence consisting of a 90 degree pulse followed by a crusher gradient to store the magnetization longitudinally and then a fast GRE readout. When the transmit gain of any given region is optimized, this sequence will result in no signal in that area. Thus, this sequence allows us to quickly scan a range of different TGs to determine the optimal TG that minimizes signal in our regions of interest. To compare the benefits of optimizing TG at 7T, we ran the 3D-CUBE sequence once with the system auto-prescan and then again after determining the optimal TG.Results
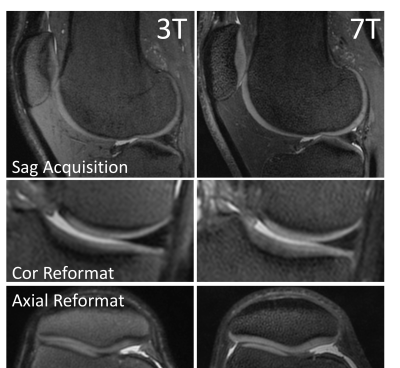
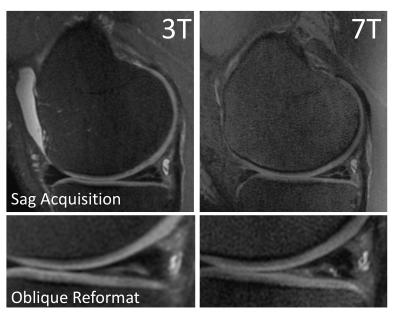
Potential benefits of 7T MRI knee scanning over 3T are shown in Figure 1. In particular, areas of shortened T2 relaxation times such as tibial cartilage and the deep layers of patellar cartilage are visualized considerably better at 7T. Further, coronal and axial reformats of high-resolution 3D-FSE-CUBE scans show less blurring at 7T compared to 3T. This is illustrated in figure 2 where oblique reformatting is able to demonstrate clearly that a meniscal tear radiates all the way through the meniscus and would require surgical repair while at 3T it is unclear. Future work would involve having MSK Radiologists compare 3T and 7T we have collected to determine whether 7T provides additional clinical information or increases diagnostic confidence.We also observed the challenges that make robust 7T imaging difficult. Figure 3 shows our manual calibration method for determining the optimal TG. The lack of signal means that TG will optimize the signal in that area while high tissue signal means poor TG for that particular area. Scanning at 3T, this is not a problem as the B1 field is fairly uniform and the MR system does a good job of correctly identifying the correct TG. However, at 7T we routinely see that the MR system determines a TG that is 10-15 decibels off of the optimal TG for the areas we are interested in clinically such as the patella-femoral and the tibio-femoral joints. This type of determined TG will cause in a 20-30% error in flip angle resulting in signal loss, blurring, and potentially even lost visualization of pathology (Figure 4). It is critical to develop methodology and training to ensure that 7T images can be correctly and robustly acquired prior to translation into clinical practice.Conclusion
Ultra-high field MR scanning at 7T provides increased resolution and SNR, allowing for isotropic imaging which can be reformatted into any scan plane to better visualize soft tissue anatomy and pathology. Using optimized TG to correct for shading and ensure flip angles of the tissue of interest provide the correction needed to overcome one challenge of 7T Imaging.Acknowledgements
GE HealthcareReferences
1. Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. 2014;95(5):986-95 e1.
2. Lovald ST, Ong KL, Lau EC, Schmier JK, Bozic KJ, Kurtz SM. Mortality, cost, and health outcomes of total knee arthroplasty in Medicare patients. J Arthroplasty. 2013;28(3):449-54.
3. Li X, Benjamin Ma C, Link TM, Castillo DD, Blumenkrantz G, Lozano J, et al. In vivo T(1rho) and T(2) mapping of articular cartilage in osteoarthritis of the knee using 3 T MRI. Osteoarthritis Cartilage. 2007;15(7):789-97.
4. Jordan CD, McWalter EJ, Monu UD, Watkins RD, Chen W, Bangerter NK, et al. Variability of CubeQuant T1rho, quantitative DESS T2, and cones sodium MRI in knee cartilage. Osteoarthritis Cartilage. 2014;22(10):1559-67.
5. Umutlu L, Ladd ME, Forsting M, Lauenstein T. 7 Tesla MR imaging: opportunities and challenges. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2014;186(2):121-9.
6. Ugurbil K. Imaging at ultrahigh magnetic fields: History, challenges, and solutions. NeuroImage. 2018;168:7-32.
Figures