DCE-MRI Characterization of Blood-Brain-Barrier Permeability Changes in Neuropsychiatric Systemic Lupus Erythematosus
Lyna Kamintsky1, Steven D. Beyea2,3, John Fisk4,5, Javeria Hashmi6, Antonia Omisade7, Timothy Bardouille8, Chris Bowen2, Maher Quraan2, Kara Matheson9, Alon Friedman1,10, and John Hanly5,11
1Department of Medical Neuroscience, Dalhousie University, Halifax, NS, Canada, 2Biomedical Translational Imaging Centre, IWK/QEII Health Centres, Halifax, NS, Canada, 3Diagnostic Radiology, Dalhousie University, Halifax, NS, Canada, 4Departments of Psychiatry, Psychology & Neuroscience and Medicine, Dalhousie University, Halifax, NS, Canada, 5Nova Scotia Health Authority, Halifax, NS, Canada, 6Department of Anesthesia, Pain Management and Perioperative Medicine, Dalhousie University, Halifax, NS, Canada, 7Acquired Brain Injury (Epilepsy Program), Nova Scotia Health Authority, Halifax, NS, Canada, 8Physics & Atmospheric Sciences, Dalhousie University, Halifax, NS, Canada, 9Research Methods Unit, Nova Scotia Health Authority, Halifax, NS, Canada, 10Department of Physiology and Cell Biology, Ben-Gurion University of the Negev, Beer Sheva, Israel, 11Department of Medicine and Division of Rheumatology, Dalhousie University, Halifax, NS, Canada
1Department of Medical Neuroscience, Dalhousie University, Halifax, NS, Canada, 2Biomedical Translational Imaging Centre, IWK/QEII Health Centres, Halifax, NS, Canada, 3Diagnostic Radiology, Dalhousie University, Halifax, NS, Canada, 4Departments of Psychiatry, Psychology & Neuroscience and Medicine, Dalhousie University, Halifax, NS, Canada, 5Nova Scotia Health Authority, Halifax, NS, Canada, 6Department of Anesthesia, Pain Management and Perioperative Medicine, Dalhousie University, Halifax, NS, Canada, 7Acquired Brain Injury (Epilepsy Program), Nova Scotia Health Authority, Halifax, NS, Canada, 8Physics & Atmospheric Sciences, Dalhousie University, Halifax, NS, Canada, 9Research Methods Unit, Nova Scotia Health Authority, Halifax, NS, Canada, 10Department of Physiology and Cell Biology, Ben-Gurion University of the Negev, Beer Sheva, Israel, 11Department of Medicine and Division of Rheumatology, Dalhousie University, Halifax, NS, Canada
Synopsis
This educational talk is aimed at MR physicists looking to gain an introductory background to neuropsychiatric systemic lupus erythematosus (NPSLE), the role of neuroinflammation in dysfunction of the blood-brain barrier (BBB) in NPSLE, and specifically the role of Dynamic Contrast Enhanced MRI (DCE-MRI) in evaluating diseases/disorders such as NPSLE.
Target Audience:
MR physicists looking to gain an introductory background to neuropsychiatric systemic lupus erythematosus (NPSLE), the role of neuroinflammation in dysfunction of the blood-brain barrier (BBB) in NPSLE, and specifically the role of Dynamic Contrast Enhanced MRI (DCE-MRI) in evaluating diseases/disorders such as NPSLE.Objectives:
To provide a basic understanding of (i) current concepts of the immunopathogenesis of NPSLE, (ii) the existing pre-clinical and clinical evidence for BBB dysfunction in NPSLE, and (iii) DCE-MRI methodology for characterizing BBB dysfunction in diseases such as NPSLE (and others) and how this differs from conventional DCE-MRI methods used in cancer imaging.Purpose:
The occurrence of neuropsychiatric (NP) events in patients with SLE is incompletely understood and frequently presents a diagnostic challenge in the attribution of NP events to SLE or other causes [1]. The immunopathogenic pathways and associated clinical NPSLE manifestations may be ischemic (causing focal disease such as stroke) or inflammatory (causing diffuse disease such as psychosis) [2]. Inflammatory NPSLE disease may be associated with changes in BBB permeability. As clinical NPSLE events are poorly correlated with conventional neuroimaging of structural abnormalities, the use of functional neuroimaging is of interest [2-3]. Recently, DCE-MRI has been used to characterize changes in slow rate BBB leakage in clinical populations such as individuals with mild traumatic brain injury and bi-polar disorder [4-6]. In this presentation, we will explore whether DCE-MRI may be used to identify patients with NPSLE.Methods:
DCE-MRI is most commonly used in studies of cancer to examine focal alterations in permeability that lead to rapid uptake of a contrast agent over approximately 5-minute time scales. Dysfunction of the BBB is also associated with a variety of neurologic disorders, particularly those with a neuroinflammatory cause. Methodology for characterizing more subtle changes in BBB permeability – i.e. slow contrast agent uptake over approximately 30-minute time scales – has been demonstrated in published studies of various neurological diseases. To-date there is limited evidence for BBB leakage in SLE patients, in spite of SLE being a systemic inflammatory disease [7-9]. We hypothesized that DCE-MRI would provide objective evidence of BBB leakage in patients with NPSLE.Results & Discussion:
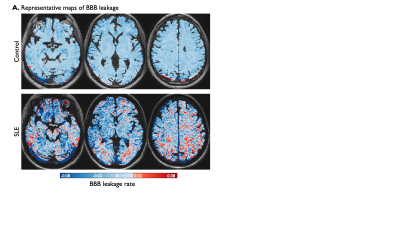
Representative DCE-MRI maps of BBB permeability in a healthy control and a patient with NPSLE are shown in Figure 1. This DCE-MRI data was acquired following injection of 0.1 mmol/kg of gadobenate dimedlumine, with voxel-wise analysis as described by Chassisim et al (2013), for contrast accumulation during the slow enhancement period 6-20 minutes post-injection [10-11]. Extensive BBB dysfunction has been shown to be associated with more frequent cognitive deficits [5, 12]. In NPSLE patients this may occur because peripheral autoimmune and inflammatory activity enhances BBB permeability, which then induces neuroinflammatory changes and associated alterations in the function of neuronal networks.Conclusion:
DCE-MRI data acquired during the slow enhancement period can reveal patterns of subtle BBB leakage. BBB dysfunction induces a neuroinflammatory response, which further enhances permeability, and has been observed in a variety of clinical pathologies, revealing both focal (e.g, stroke, TBI) and diffuse (e.g. bipolar, aging) BBB leakage. It may also be an objective biomarker in NPSLE.Acknowledgements
This work was supported by a grant from the Canadian Institutes for Health Research, and scholarship funding from Mitacs.References
- Kello N. et al “Cognitive Dysfunction in Systemic Lupus Erythematosus: A Case for Initiating Trials” Arthritis & Rheumatology 71(9), 1413-1425 (2019).
- Hanly J.G et al “Nervous System Disease in Systemic Lupus Erythematosus: Current Status & Future Directions” Arthritis & Rheumatology 71(1), 33-42 (2019).
- Postal M. et al “Magnetic resonance imaging in neuropsychiatric lupus erythematosus: current state of the art and novel approaches” Lupus 26, 517-521 (2017).
- Wessberg I. et al “Imaging Blood-Brain-Barrier Dysfunction in Football Players” JAMA Neurology 71(11), 1453-1455 (2014).
- Kamintsky L. et al “Blood-brain barrier imaging as a potential biomarker for bipolar disorder progression” Neuroimage: Clinical, in press, October 22 (2019).
- Veksler R. et al “Slow blood-to-brain transport underlies enduring barrier dysfunction in American football players” Brain, accepted (2020).
- Abbott N. et al “The blood-brain barrier in system lupus erythematosus” Lupus 12(12), 908-915 (2003).
- Chi JM et al “Alterations in blood-brain barrier permeability in patients with systemic lupus erythematosus. American Journal of Neuroradiology” 40(3), 470-477 (2019).
- Wagsul ME et al “Dynamic contrast enhancement in a mouse model of neuropsychiatric system lupus erythematosus” Proc Intl Soc Magn Reson Med, 12:2861 (2013).
- Veksler R. et al “Blood-brain barrier in human neuropathologies” Arch. Med. Res. 45, 646-652 (2014).
- Chassisim et al “Quantitative imaging assessment of blood-brain barrier permeability in humans” Fluids Barriers CNS 10:9 (2013).
- Kaminitsky L. et al “Blood-Brain Barrier Imaging as a Biomarker for Cognitive Decline in Systemic Lupus Erythematosus” Proc. Intl Soc Magn Med, 2480 (2020).