Contrast Agents
Scott Reeder1
1Radiology, University of Wisconsin, Madison, WI, United States
1Radiology, University of Wisconsin, Madison, WI, United States
Synopsis
Contrast agents are an indispensable tool that can be used to improve the detection and characterization of a plethora of diseases, in a wide variety of clinical and research applications. GBCAs are the most widely used agents with tremendous experience over the last 30 years. Despite their outstanding safety records, safety concerns NSF and gadolinium deposition warrant attention in the literature as this subject evolves. Attention to optimization of pulse sequences to best exploit the use of contrast agents for disease detection should always be considered and can bear great fruit for maximizing the benefit of contrast with clinical MRI.
Highlights
- Contrast agents are an indispensable tool with many clinical and research applications in MRI.
- This talk will review the mechanisms by which contrast is used including principles of T1 and T2 relaxivity.
- The factors used to choose a contrast agent is complex, and typically involves considerations such as relaxivity, pharmacokinetics, cost, and safety.
- There are only two generally accepted safety considerations when gadolinium-based contrast agents: i) acute adverse reactions/ anaphylactoid reactions and ii) nephrogenic systemic fibrosis.
- Maximizing image quality through the use of optimized pulse sequences is important, in order to maximally exploit the benefit of contrast agents.
Why Do We Need Contrast Agents?
MRI is a rich imaging modality with a plethora of contrast mechanisms that can be used for accurate diagnosis of a variety of diseases. With this incredible armamentarium of contrast mechanisms that include T1, T2 diffusion weighting, blood flow, oxygen sensitive imaging, iron and fat sensitive imaging, among many others, why is it that we need to supplement MRI with exogenous contrast agents? Although many MRI exams can be performed without the use of exogenous contrast, contrast agents can provide dramatic alterations in soft tissue contrast with increased signal to noise ratio (SNR) performance, improved conspicuity of more subtle pathology not visible with non-contrast MRI techniques, and even quantitative information. Contrast agents can be used to improve the detection and delineation of a variety of cancers, heart disease, depiction of subtle vascular abnormalities, and can even be used to provide quantitative information such as blood flow and tissue perfusion, among others. Characterization of liver tumors as benign versus malignant as well as functional information in a variety of organs can only be made possible with the addition of contrast agents. The list of applications is too long to list in this syllabus and in this lecture, but a few illustrative examples will be provided. Needless to say, exogenous contrast agents are an indispensable agents for many clinical MRI exams. In this lecture and this syllabus, I will provide a review of how contrast agents work, how to characterize contrast agents and their overall efficacy, including the concept of “relaxivity”, the importance of pharmacokinetics, and other important considerations including cost and safety related issues. Further, we will discuss how to optimize pulse sequences to best exploit a contrast agent to maximize image quality, SNR, and contrast to noise ratio (CNR) between normal and abnormal tissue, or other tissue of interest. Finally, we will briefly touch on established and emerging safety related issues including allergic and acute adverse reactions, nephrogenic systemic fibrosis (NSF), gadolinium deposition phenomenon, and “gadolinium deposition disease”.What is Contrast and How Does it Work?
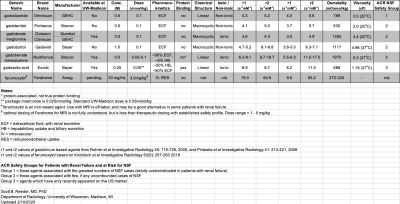
There are a number of paramagnetic substances that have been demonstrated to accelerate the relaxation times of protons as they relax back towards equilibrium. Specifically, these agents will accelerate the rate of longitudinal relaxation by shortening the T1, as well as enhancing the relaxation of transverse magnetization by shortening the T2and T2* signal decay. The lanthanide rare earth metals are the most notable agents, as well as other paramagnetic elements, such as iron, manganese, and even oxygen. The most commonly used agent is gadolinium, administered in a chelated form in order to avoid toxicity of a free gadolinium salt. Other rare earth metals that have been used experimentally in MRI include europium and dysprosium. Other paramagnetic metals such as manganese have shown tremendous potential as a contrast agent. Finally, iron oxide-based agents, usually in the form of superparamagnetic iron oxides (SPIOs) have emerging applications, particularly for angiography and cell tracking.Gadolinium-based contrast agents (GBCAs) are by far the most important and widely used contrast agents for MRI. As shown in Table 1, there are currently six GBCA agents on the market. There are a variety of characteristics that differentiate these agents from one another, related to the molecule used to chemically isolate (i.e. chelate), the gadolinium ion from the body. Key characteristics include the formulation or concentration. Most agents are formulated at 0.5M (“half molar”), although some agents are as low as 0.25M and range up to 1.0M. Classically, the typical dose for early GBCAs was 0.1 mmol/kg, although newer agents can be administered at lower doses, as low as 0.025 mmol/kg. As described below, there are important differences in the pharmacokinetics of these agents as well as the chemical structure which may have safety considerations. Some agents are ionic or nonionic which is a major consideration for iodinated contrast agents, but of less importance for GBCAs. Osmolality and viscosity are also minor considerations, given the relatively low volumes administered and the relatively low viscosity of GBCAs compared to iodinated contrast agents.
How do I Choose a Contrast Agent?
There are multiple considerations to this challenging proble$$m. I have grouped these considerations into: i) relaxivity, ii) pharmacokinetics, iii) cost, and iv) safety. The relative importance of these considerations may depend on the specific application and other patient considerations.1. Relaxivity: Relaxivity is the “bang for your buck” of a contrast agent and describes the amount of T1, T2*, or T2 shortening obtained per molecule of a contrast agent. The formula is as follows:
$$R_1=R_1^o + r_1[C]$$
where the R1 (=1/T1) is the longitudinal relaxation rate after the administration of a contrast agent with concentration [C] and longitudinal “relaxivity” r1, and is the relaxation rate before the administration of contrast. Similar expressions can be written for R2 and R2* relaxivity. Thus, for a given dose of contrast, the higher the r1,r2, and r2*, will determine the efficacy of the contrast agent. Detailed measurements of the relaxivity of various contrast agents are shown in Table 1. The relaxivity of an agent depends on many things, including the molecular size of the agents, field strength, and biological environment where the agent can interact with large molecules in the body. In general, the larger the molecule, or any interaction with molecules in the environment that slows the tumbling rate of the contrast agent, the higher the relaxivity.
As a general rule of thumb, most contrast-enhanced imaging is performed with T1-weighted imaging, and therefore the r1 is typically the most important relaxation parameter. It is for this reason that high relaxivity agents such gadobenate dimeglumine and gadobutrol have obtained significant interest, given their superior T1shortening compared to other agents, for the same dose of contrast. The higher relaxivity also offers an opportunity to reduce the dose of contrast for similar levels of contrast enhancement.
2. Pharmacokinetics: Historically, first generation GBCAs were extracellular fluid agents, that is they had similar pharmacokinetics to iodinated contrast agents where they would be injected intravenously, remain within the blood pool for a short period of time but extravasate into the interstitial space, particularly within tissues such as tumors with high volumes of distribution. This provided the basis for enhancement of abnormal tissue such as tumor, inflammation, or scar.
More recently, particularly with the advent of gadoxetic acid, hepatobiliary uptake through the organic anion transporter polypeptide (OATP) into hepatocytes, and a subsequent excretion into bile has led to significantly new and important opportunities for hepatobiliary imaging. This provides not only increased detection of tumors of non-hepatocyte origin, but also improved characterization of primary hepatic tumors as benign vs malignant. T1-weighted MR cholangiography has led to important applications in biliary imaging such as strictures, bile leaks, and other biliary pathology. Some contrast agents such as gadobenate dimeglumine have a small degree of hepatobiliary excretion which can be used to similar effect.
Ferumoxytol, a SPIO available on the market for treatment of anemia, has demonstrated tremendous interest as an off-label use with MRI. Ferumoxytol is an intravascular agent for the first 10-20 hours after injection, with strong T1 shortening effects and has shown great promise as an intravascular agent for MR angiography and MR venography. Over a span of several days, ferumoxytol is taken up into the reticuloendothelial system (RES), most notably the liver, spleen, bone marrow, and to a lesser extent lymph nodes. This offers useful opportunities to characterize abnormalities of these organs. For example, differentiation of pancreatic neuroendocrine tumor from intrapancreatic splenule can be performed through the administration of ferumoxytol. Splenules have uptake that matches that of the spleen and can be used to exclude a potentially malignant pancreatic tumor.
3. Cost: There is variability in the cost of various contrast agents. Depending on the specific application, high relaxivity or specialized pharmacokinetics may be more or less important and thus cost is an important consideration in order to deliver cost effective imaging care. For applications that do not require specialized pharmacokinetics or high relaxivity, an older, less expensive agent may suffice.
4. Safety: Please see below for special considerations on safety that may impact the choice of contrast agent.
Safety Considerations
Safety considerations for GBCAs can be broken down into four general categories:1. Allergic or immediate acute adverse reactions: While not well understood, acute adverse reactions and/or anaphylactoid reactions are, by far, the most important adverse effect of GBCAs. Acute reactions can occur with any medication, and are common with iodinated contrast agents. Although GBCAs are extraordinary safe and contrast reactions are very uncommon, they do occur, rarely with life threatening consequences. By far, the most important risk of GBCAs are acute adverse actions, dwarfing the overall morbidity and mortality of any other adverse effect of GBCAs. There are important differences in the safety profiles of GBCAs and large retrospective studies have been published. In general, linear contrast agents, most notably gadodiamide, are generally considered to have the best safety profile from the perspective of acute adverse reactions. Other agents tend to have a higher rate of adverse reactions to gadolinium, including macrocyclics. Overall it should be noted, that despite these differences, all GBCAs on the market are generally regarded as extraordinarily safe.
Importantly, ferumoxytol has been associated with deaths linked to hypotension during bolus injection of ferumoxytol. For this reason, the administration of ferumoxytol should be include dilution and infusion over a 15-minute period. Guidelines on the safe administration of ferumoxytol for us with MRI have been published (Vasanawala et al MRM 2016 75(5): 2107-11). I also note that weight-based doses used for MRI (eg. 3-7mg/kg) are generally much lower than therapeutic doses (510mg).
2. Nephrogenic systemic fibrosis: NSF was first described in the mid-2000s as a severe debilitating disorder characterized by skin thickening, joint contractures, and systemic fibrosis, occurring in patients with renal failure who have been exposed to certain GBCAs. Although NSF is not well understood, the evidence linking GBCAs and renal failure is strong. Patients who have renal failure (eGFR <30, or on dialysis) are considered at greater risk and such patients should avoid GBCAs where possible. There is only one agent available on the market (gadodiamide) that has been associated with NSF. No other agent on the market has been clearly linked to NSF. For these reasons, the American College of Radiology (ACR) has created three safety groups. Group 1 agents, which only includes gadodiamide, should be avoided in those patients with renal failure. Group 2 agentsinclude gadobenate dimeglumine, gadoteridol, gadoterate dimeglumine, and gadobutrol, and are generally regarded as safe if a GBCA-enhanced MRI exam is required. Gadoxetic acid is a Group 3 agent, which classifies it as an agent of uncertain potential to lead to NSF. It has never been associated with NSF but it has a shorter duration on the market and few exposures in patients with renal failure, and thus its safety with regards to NSF risk in indeterminate at this time. Ferumoxytol, which does not contain gadolinium, is generally regarded as safe in patients with renal failure.
3. Gadolinium deposition phenomenon: In 2014 Kanda et al published a landmark paper reporting the subtle but definite increase in signal density in certain deep regions of the brain on T1-weighted MRI prior to the administration of contrast, in patients who have received multiple past doses of contrast. Since then there has been numerous publications demonstrating a dose dependent deposition of GBCAs in the brain, skin, bone, and other tissues. While the data are incomplete and much work remains to be done, it is clear that all GBCAsdeposit tiny amounts of gadolinium in the body. Fortunately, no clinical or biological consequences, have been reported from this deposition, and therefore the clinical implications, if any, remain unknown. Despite the lack of any biological or clinical data demonstrating any harm from deposited gadolinium, the FDA and other agencies have issued black box warnings to make the public aware of this phenomenon. Continued research, including prospective human and animal studies, are ongoing. As stated at the FDA MIDAC Meeting in September 2017, the FDA determined that GBCAs are extraordinarily safe and that the risk related to gadolinium deposition, while unknown, is far offset by the proven clinical benefits of GBCAs for diagnosis and treatment monitoring of a large number of diseases. The literature on the gadolinium deposition phenomenon continues to evolve.
4. “Gadolinium Deposition Disease”: “GDD” is a term coined in recent years by one group of authors who have reported idiopathic reactions to the administration of gadolinium, in the absence of renal failure (Semelka et al AJR 2016 207(2): 229-33). The symptoms of “GDD” are not clearly linked to NSF and the etiology and relationship to the administration of gadolinium is unknown. At this time, “GDD” is not an accepted entity and is not substantiated by any scientific or clinical data. Nonetheless, anecdotal reports should be taken seriously and this may be a subject that continues to involve in coming years. At this time, however, “GDD” should not be recognized as an established safety risk of GBCAs.