MRI without Sedation & Anesthesia. Are we there yet?
1Children's Hospital of Philadelphia, United States, 2Radiology, Ohio State University, Columbus, ON, United States, 3Nationwide Children's Hospital, Columbus, OH, United States, 4Radiology, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States
Synopsis
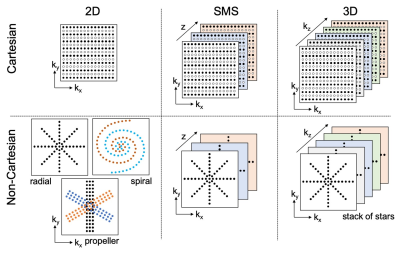
Newer motion robust acquisition methods are now available that have the potential to significantly minimize or remove the need for sedation and anesthesia in abdominal imaging. These new acceleration and motion robust MR techniques allow for free-breathing abdominal MRI and should allow for a decrease in MR scan times and sedation requirements. Familiarity with the advantages and trade-offs of these methods is essential for the radiologist performing the optimal study and for guiding the technologist acquiring the MR images.
Objective: In this presentation, we intend to review established and emerging methods for reducing motion artifacts in an attempt to move towards sedation/anesthesia-free MRI.
Conclusion: We intend to clearly understand the strengths and limitations of motion reduction methods that can enable practitioners of pediatric MRI to select and combine the appropriate techniques and potentially minimize the need for sedation and anesthesia.
Acknowledgements
n/aReferences
1. Chandarana H, Block TK, Rosenkrantz AB, et al. Free-breathing radial 3D fat-suppressed T1-weighted gradient echo sequence: a viable alternative for contrast-enhanced liver imaging in patients unable to suspend respiration. Invest Radiol.
2. Feng L, Benkert T, Block KT, Sodickson DK, Otazo R, Chandarana H. Compressed sensing for body MRI. Journal of magnetic resonance imaging : JMRI. 2017.
3. Morin CE, Dillman JR, Serai SD, Trout AT, Tkach JA, Wang H. Comparison of Standard Breath-Held, Free-Breathing, and Compressed Sensing 2D Gradient-Recalled Echo MR Elastography Techniques for Evaluating Liver Stiffness. AJR American journal of roentgenology. 2018
Figures