4851
Quantitative T2 Mapping in Advanced Cervical Cancer: A Pilot Study of Patients’ Concurrent Chemoradiotherapy Response1Department of Magnetic Resonance, the First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 2MR Collaboration, Siemens Healthcare Ltd, Beijing, China, 3MR R&D Collaboration, Siemens Healthineers, Los Angeles, CA, United States
Synopsis
This study determined the value of quantitative transverse relaxation time (T2) mapping as an alternative method to conventional magnetic resonance imaging (MRI) for evaluating the response to concurrent chemoradiotherapy (CCRT) in 27 patients with advanced cervical cancer (CC). Response values were calculated at three time points (before CCRT, 4 weeks after CCRT, and at the end of CCRT) and then compared. The results showed that quantitative T2 mapping can be effectively used for monitoring treatment response during and after treatment, but not for pre-treatment monitoring.
Purpose
Concurrent chemoradiotherapy (CCRT) is a current standard treatment protocol for advanced cervical cancer (CC) [1]. Additionally, magnetic resonance imaging (MRI) is widely used for monitoring treatment response in CC patients undergoing CCRT. However, the accuracy of conventional MRI techniques (morphologic T2-weighted sequences) alone in monitoring treatment response has yielded poor results historically [2, 3]. Therefore, this study aimed to investigate quantitative transverse relaxation time (T2) mapping as an improved alternative method for assessing the treatment response of advanced CCs to CCRT.Materials and Methods
Twenty-seven patients diagnosed with advanced CC underwent conventional MRI and quantitative transverse relaxation time (T2) mapping on a 3T system (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) at 3 intervals: prior to receiving CCRT (T2-pre), in the beginning of the 4th week of CCRT (T2-mid), and immediately after CCRT completion (T2-post). Patients were classified according to the Response Evaluation Criteria in Solid Tumors (RECIST) after CCRT as to having a complete response (CR group, n = 17) or partial response (PR group, n = 10). The T2 maps were estimated based on the T2-weighted images acquired using a Radial Turbo Spin Echo–based prototype sequence (Siemens Healthcare, Erlangen, Germany) with the following parameters: TR/TE = 5720/22, 33, 44, 55, 66, 77, 88, 99ms; FOV = 220×220mm2; slice thickness = 4mm; voxel size = 0.8×0.8×4.0 mm3; 20 slices; flip angle = 145°; acquisition time = 4 min. The T2 values at each time point (T2-pre, T2-mid, and T2-post) and the T2 percentage of change at adjacent time points (ΔT2-mid and ΔT2-post) were obtained. The Mann-Whitney U test was used to compare the differences in T2 values and the percentage of change between the response group and the non-response group. Diagnostic performance was evaluated based on measurements calculated via a receiver operating characteristic curve (ROC) analysis. A P value of <0.05 was considered to indicate a statistically significant difference.Results
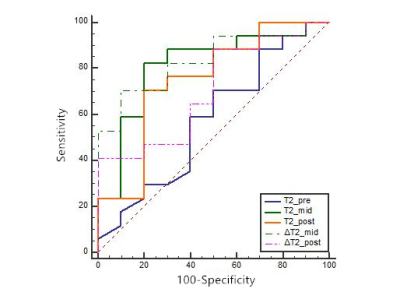
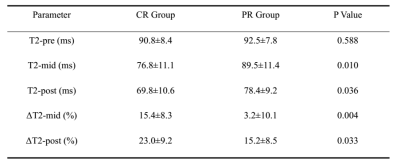
Both the T2-mid and T2-post values of the CR group were lower than those of the PR group (P = 0.010 and P = 0.036, respectively). The CR group showed greater ΔT2-mid and ΔT2-post values (P = 0.004 and P = 0.033, respectively). No significant difference was found in the T2-pre values between the two groups (P = 0.588). The T2 values obtained from the CR group and PR group are shown in Figure 1. The ROC analysis yielded area under the curve (AUC) values of 0.574, 0.812, 0.747, 0.835 and 0.706 for T2-pre, T2-mid, T2-post, ΔT2-mid, and ΔT2-post, respectively, for predicting the complete response of advanced cervical cancer to CCRT. The optimum threshold for T2-mid and ΔT2-mid was 81.3 ms and 7.7%, resulting in a sensitivity of 82.4% and 90.0%, respectively, and a specificity of 80% and 70.6%, respectively. Figure 2 shows image examples from 2 patients, and Figure 3 shows the ROC curves of all 5 parameters.Discussion
In this study, we investigated dynamic changes in T2 values following CCRT in patients with advanced CC. We found that the tumor response (CR or PR) was associated with a decrease of T2 values during CCRT. Our study showed that, except for T2-pre, all values (T2-mid, T2-post, ΔT2-mid and ΔT2-post of the CR group) were significantly different from those of the PR group. The results suggest that quantitative T2 values hold the potential for effective monitoring of the CC response to CCRT. Moreover, T2-mid and ΔT2-mid were more sensitive than T2-post and ΔT2-post for predicting complete response of advanced CC to CCRT.Conclusion
It is feasible to use quantitative T2 values and percentage T2 change during CCRT to monitor treatment response, especially during early treatment response in patients with advanced cervical cancer.Acknowledgements
The authors have no acknowledgements.References
[1] National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology. CC, Version I.2019. Volume 2018. Plymouth Meeting: National Comprehensive Cancer Network; 2018.
[2] Thomeer MG, Vandecaveye V, Braun L, et al. Evaluation of T2-W MR imaging and diffusion-weighted imaging for the early post-treatment local response assessment of patients treated conservatively for cervical cancer: a multicentre study. Eur Radiol 2019;29:309-318.
[3] Yang W, Qiang JW, Tian HP, et al. Multi-parametric MRI in cervical cancer: early prediction of response to concurrent chemoradiotherapy in combination with clinical prognostic factors. Eur Radiol 2018;28:437-445.
Figures
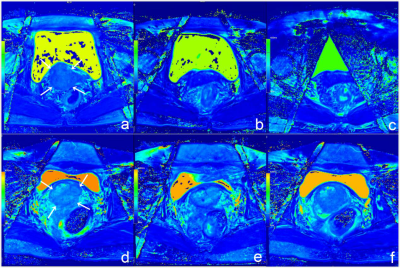
(a-c) T2 maps of a 68-year-old CC patient with CR. T2 maps showed a cervical mass before therapy (arrows) (a), which reduced in size markedly 4 weeks after CCRT (b) and at the end of CCRT (c). The T2 values of the lesion were 86.3 ms, 80.1 ms and 63.7 ms, indicating a substantial decrease.
(d-f) T2 maps of a 47-year-old CC patient with PR. T2 maps show a cervical mass (arrows) (d), which decreased in size slightly 4 weeks after CCRT (e) and at the end of CCRT (f). The T2 values of the lesion were 97.0 ms, 105.2 ms and 93.5 ms, not indicating a substantial decrease.